Cleft Lip and Palate
What is cleft lip and palate
Cleft lip and palate are birth defects of the lip and mouth, also known as orofacial clefts. Very early in pregnancy, a developing fetus has a split lip and palate, but around seven weeks of gestational age, the sides of the lip and the roof of the mouth should fuse. Failure of fusion results in cleft lip and/or cleft palate.
- About 6,000 to 8,000 kids are born in the United States with orofacial clefts every year. The worldwide incidence of cleft lip with or without cleft palate is 1 in 700 births.
- Cleft defects are more common in boys
- Cleft defects are more common in specific ethnic backgrounds such as Asians and certain groups of American Indians or Alaska Natives and are less common in African-Americans
- Less than 13 percent of patients have other birth defects
What is cleft lip?
Cleft lip is an abnormality in which the lip does not completely form during fetal development. The degree of the cleft lip can vary greatly, from mild (notching of the lip) to severe (large opening from the lip up through the nose), in which case the cleft can be very noticeable.
What is cleft palate?
Cleft palate occurs when the roof of the mouth does not completely close during fetal development, leaving an opening that can extend into the nasal cavity. It can extend from the front of the mouth (hard palate) to the throat (soft palate). Often the cleft in palate will also include the lip.
Cleft palate is not as noticeable as cleft lip because it is inside the mouth. Children can also have a less noticeable form of cleft palate, known as a submucous cleft palate. This is a cleft covered by the mucous membrane that lines the roof of the mouth.
Children can have only a cleft lip, only a cleft palate or a cleft lip and palate. These anomalies can be isolated or syndromic in nature. Often, there is a family history of cleft lip or palate.
Watch our educational video to learn more about the diagnosis and treatment of cleft lip and palate.
What are the different types of cleft lip and palate?
The different types of cleft defects are categorized according to the location of the cleft and how much of the lip is involved:
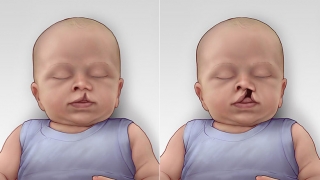 Unilateral incomplete (on left) and complete (on right) cleft lip
Unilateral defects – the most common type of cleft, affecting one side of the lip, with or without a cleft palate
Unilateral incomplete (on left) and complete (on right) cleft lip
Unilateral defects – the most common type of cleft, affecting one side of the lip, with or without a cleft palate
- Incomplete unilateral cleft lip and/or palate – a notching of the lip that does not extend into the nose, may be accompanied by a cleft palate
- Complete unilateral cleft lip and/or palate – an opening that extends from one side of the lip into the nose and/ may be accompanied by a cleft palate
 Bilateral incomplete (on left) and complete (on right) cleft lip
Bilateral defects – affecting both sides of the lip and/or palate, forming two clefts
Bilateral incomplete (on left) and complete (on right) cleft lip
Bilateral defects – affecting both sides of the lip and/or palate, forming two clefts
- Incomplete bilateral cleft lip and/or palate – a notching of both sides of the lip that does not extend into the nose, may be accompanied by a cleft palate
- Complete bilateral cleft lip and/or palate – an opening that extends from both sides of the lip into both nostrils. may be accompanied by a cleft palate
- Children can also have less noticeable form of cleft lip than those depicted above, known as a form-fruste cleft lip. A form-fruste cleft lip is a small, subtle indentation of the lip.
Causes
The cause of cleft lip and palate is not completely understood, though we know that a combination of genetic and environmental factors contribute to cleft lip and palate.
In addition, there are several syndromes that are commonly associated with cleft lip and palate. These conditions may have features that are able to be detected on prenatal imaging, and can be tested for pre- or postnatally with help of a board-certified genetic counselor.
- Van der Woude syndrome
- Stickler syndrome
- Pierre Robin sequence or syndrome
- Hemifacial microsomia
- Goldenhar syndrome
- Downs syndrome
- CHARGE syndrome
- 22q and velocardiofacial syndrome
- DiGeorge syndrome
- Oro-mandibular limb hypoplasia syndrome
- Opitz syndrome
Recurrence risk, or chance that a future baby also has a cleft lip or palate, can vary depending on family history, etiology and associated anomalies. If a family has no prior family history and has a baby with a cleft without an identified cause the recurrence risk ranges from 2-8%.
Complications
Beyond the cosmetic difference, children born with an orofacial cleft are at risk for other possible complications after birth. Our Cleft Lip and Palate Program brings together a team that specializes in providing treatment and long-term support for the condition and related issues.
Feeding difficulties
 Isolated cleft of the soft and hard palate, viewed from inside the mouth.
Nutrition is usually the most immediate concern for a baby with a cleft palate. Sucking is difficult for a child with cleft palate because the roof of the mouth is not formed completely. This makes it difficult for a baby to create enough suction to pull milk from a standard bottle or the breast. A baby may appear to be working very hard at feeding but end up taking only a very small amount of breast milk or formula. When this happens, the baby does not gain weight properly. Feeding difficulties occur more with cleft palate. Children with cleft lip only do not usually have feeding difficulties.
Isolated cleft of the soft and hard palate, viewed from inside the mouth.
Nutrition is usually the most immediate concern for a baby with a cleft palate. Sucking is difficult for a child with cleft palate because the roof of the mouth is not formed completely. This makes it difficult for a baby to create enough suction to pull milk from a standard bottle or the breast. A baby may appear to be working very hard at feeding but end up taking only a very small amount of breast milk or formula. When this happens, the baby does not gain weight properly. Feeding difficulties occur more with cleft palate. Children with cleft lip only do not usually have feeding difficulties.
Issues of extra air intake and nasal regurgitation (milk coming from the nose) may also occur. With proper teaching, support and patience, most babies with cleft palate go on to do very well with feeding. In some cases, extra support from a feeding team may be recommended. Children’s Hospital has resources that can help with feeding a baby with a cleft palate.
Ear infections and hearing loss
Patients with a cleft palate are more susceptible to ear infections. The muscles of the palate have an important role in draining fluid from the inner ear. When a cleft palate is present this fluid does not drain normally and can become infected.
Recurrent infections can lead to hearing loss, so patients with cleft palate are often seen by an otolaryngologist (ear, nose and throat specialist) who may recommend the surgical placement of ventilating tubes in the eardrum. Ear tubes can prevent fluid build-up and lessen the occurrence of ear infections and associated hearing loss. These tubes are often placed at the time of cleft lip or palate repair and may need to be replaced as necessary to preserve normal hearing.
Speech and language delay
Due to the opening of the roof of the mouth and the lip, muscle function may be decreased, which can lead to delayed or abnormal speech. Referral to a speech therapist should be discussed with the child’s physician.
Proper speech is dependent upon many factors, but the most common problems associated with cleft lip and palate are related to articulation and nasal escape during speech. Nasal escape may be caused by a short palate or by palate dysfunction due to problems with the palatal muscle. Patients significantly impacted by palatal insufficiency (also called velopharyngeal insufficiency) may require secondary procedures and can be treated in coordination with our Velopharyngeal Dysfunction Program.
Cosmetic deformity
As the child grows, they might develop irregularities or asymmetries in the face, either due to clefting or abnormal facial growth. We can help with appearance concerns.
Upper and lower jaw discrepancy
Some children with cleft lip and palate have jaws that grow at different rates, sometimes leading to difficulties with chewing food, improper alignment of teeth, and even early jaw-joint arthritis. Our team specializes in treating these issues.
Difficulties with nasal breathing
It is not uncommon for children born with a cleft lip to have a deviated septum, a problem that can make it difficult to breathe out of both sides of the nose. A septoplasty, a surgical procedure that straightens the septum, can help restore the nasal airway.
Psychosocial issues
Our specialists in pediatric psychological counseling have helped thousands of children and their families cope with the emotional and social issues that can accompany facial differences.
Dental problems
As a result of the abnormalities, teeth may not erupt normally and orthodontic treatment is usually required. The Cleft Lip and Palate Program team includes board-certified pediatric orthodontists and support from a pediatric dentist who consults with our team.
Diagnosis
 A child with unilateral cleft lip diagnosed with prenatal ultrasound
Cleft lip and palate is often diagnosed after birth, but the diagnosis can also be made prenatally. The Cleft Lip and Palate Program works closely with CHOP’s Center for Fetal Diagnosis and Treatment to provide early and accurate diagnosis, allowing our team to assess the best treatment options for each child’s unique situation. Our collaborative team focuses on:
A child with unilateral cleft lip diagnosed with prenatal ultrasound
Cleft lip and palate is often diagnosed after birth, but the diagnosis can also be made prenatally. The Cleft Lip and Palate Program works closely with CHOP’s Center for Fetal Diagnosis and Treatment to provide early and accurate diagnosis, allowing our team to assess the best treatment options for each child’s unique situation. Our collaborative team focuses on:
- Personalized attention during the pregnancy with a focus on feeding education – even before baby is born.
- Making sure families are connected with the Cleft Lip and Palate Program’s Nurse Navigator well before delivery to make for seamless care coordination between all specialists and help families prepare for what to expect.
Early diagnosis and treatment is important to achieve optimal outcomes and correction of cleft lip and palate. The discovery of cleft lip and cleft palate while a baby is still in utero allows both the family and the healthcare team to prepare, anticipate potential challenges and assemble appropriate resources to optimize the outcome for the newborn.
Cleft abnormalities are most often prenatally diagnosed around 20 weeks gestation. At this stage of fetal development, the lip and palate have normally fused, so a failure to fuse may be evident in advanced prenatal imaging tests after this time.
Prenatal evaluation
If orofacial clefting is suspected on a routine ultrasound study, expectant mothers may be referred to the Center for Fetal Diagnosis and Treatment for a comprehensive, full-day prenatal evaluation. The evaluation includes three diagnostic studies:
- A targeted, high-resolution ultrasound evaluates the extent of the cleft as well as presence of other anomalies including findings suggestive of any underlying syndrome.
- A fetal echocardiogram closely examines the structure and function of the fetal heart.
- An ultrafast fetal MRI allows for a detailed evaluation of the fetal brain, important in a case of suspected cleft lip and palate because development of the brain drives development of the face. In conjunction with ultrasound, MRI also allows for more accurate assessment of cleft palate and aids in detection of soft palate defects which can be difficult to visualize on sonography.
All families also meet with a board-certified genetic counselor who completes a detailed review of family, medical and pregnancy history, as well as discusses potential screening and diagnostic testing options that may aid in the individualized care of each child. Information from this evaluation can also assess for recurrence risk for future pregnancies.
Planning for delivery and course of treatment for cleft patients
The results of the evaluation are reviewed and families are counseled by a multidisciplinary team that includes maternal-fetal medicine specialists (MFM), reproductive geneticists, plastic and reconstructive surgeons and nurse coordinators. Individually tailored prenatal and postnatal management plans are developed in partnership with referring physicians.
If prenatal evaluation suggests a potential underlying syndrome, genetic testing may be performed through amniocentesis.
In some cases, if both mother and baby are candidates based on the initial evaluation and overall health, babies may deliver in CHOP’s Garbose Family Special Delivery Unit (SDU). By delivering in this special birthing unit located directly within CHOP, newborns have immediate access to pediatric plastic surgeons and other specialists who can assess feeding in the early hours after birth.
Diagnosis of a birth defect like cleft lip and palate is a challenging time for any family. They are currently no fetal interventions for this diagnosis. Together with other specialists from throughout the Hospital, the Cleft Lip and Palate Program and the Center for Fetal Diagnosis and Treatment provide a wide range of resources to support families throughout pregnancy, delivery, and treatment after birth.
Treatment
 Left unilateral cleft lip, after repair.
At Children’s Hospital of Philadelphia, children with cleft lip and cleft palate receive coordinated care through our Cleft Lip and Palate Program. The multidisciplinary program brings together plastic surgeons, pediatricians, orthodontists and other specialists in order to provide the most comprehensive care for every child. We also work closely with the Neonatal Craniofacial Program to manage the care of these newborns.
Left unilateral cleft lip, after repair.
At Children’s Hospital of Philadelphia, children with cleft lip and cleft palate receive coordinated care through our Cleft Lip and Palate Program. The multidisciplinary program brings together plastic surgeons, pediatricians, orthodontists and other specialists in order to provide the most comprehensive care for every child. We also work closely with the Neonatal Craniofacial Program to manage the care of these newborns.
The surgical procedures required for each patient with cleft lip and palate will vary depending upon the type and severity of the deformity. Timing and treatment will be adjusted based on each patient’s overall medical needs, but treatment typically includes a combination of the following procedures and stages, performed within general time frames based on development.
- Nasoalveolar molding (NAM) (1 week to 3 months of age, if needed)
- Cleft lip repair (3 to 6 months)
- Cleft palate repair (9 to 18 months)
- Palatal expansion (5 to 7 years, if needed)
- Alveolar bone graft and fistula repair (6 to 9 years)
- Tip rhinoplasty (6 to 9 years)
- Phase I orthodontics (6 to 9 years)
- Phase II orthodontics (14 to 18 years)
- Orthognathic surgery (jaw surgery) (14 to 18 years)
- Final touchup surgery (adolescence or adulthood)
Learn more about what to expect during the course of cleft lip and palate treatment »
Long-term care
After successful surgical repair of cleft lip and/or cleft palate, Cleft Lip and Palate Program patients will return to our clinic for yearly appointments that will include meetings with specialists, an overall health assessment, and surgical follow-up. Once a patient has reached maturity and completed all of the procedures and treatment, they are generally discharged from annual clinic visits.
From the moment your child enters our program, our multidisciplinary team partners with your pediatrician or primary care physician to provide coordinated care, making treatment recommendations according to each patient’s unique needs.
Our program brings together a variety of pediatric specialists, all with extensive experience treating children with cleft lip and palate. Your child’s long-term care will include:
Surgical follow-up
Your plastic surgeon will monitor for potential complications (such as formation of fistulas or openings of palate into nose) to determine if any additional palatal procedures are needed. Because the nature of cleft lip and palate makes it possible that a patient will require surgery later in life, we continue to follow our patients in the long term.
Speech and language assessments
Shortly after birth, a speech and language pathologist will evaluate your child’s feeding skills and oral-motor development to determine the need for any specific treatment or procedures. In the early years, our team will partner with your pediatrician to monitor for delays in speech and language development, and make any appropriate referrals for early intervention.
Around 3 years of age, when children have the ability to follow directions and speak in sentences, we begin yearly speech and language evaluations during clinic visits to assess palatal function. Due to changes in the growth of the face and oral structures as your child grows, routine evaluations continue through the teen years to monitor language development, articulation and vocal quality.
Our internationally recognized speech pathologists work with your plastic surgeon, orthodontist and dentist to plan individualized treatment needed to improve your child’s communication skills and make recommendations for speech therapy or surgery as needed.
Audiology assessments
A hearing specialist will provide periodic reports that are used in coordination with evaluations by an ear, nose and throat (ENT) specialist to care for repeated ear infections or hearing loss that frequently accompany cleft palate. The ENT specialist may recommend the surgical placement of ventilating tubes in the eardrum to prevent fluid build-up and lessen the occurrence of infections and hearing loss.
Dental and orthodontic care
Our dental and orthodontic specialists keep track of your child’s dental growth and development, making recommendations regarding proper care for developing teeth, as well as the timing of any necessary surgical procedures or corrective orthodontics. Our specialists will partner with your primary care physicians and other specialists to meet each patient’s dental and orthodontic needs.
Psychosocial counseling and support
A dedicated psychologist is available to evaluate patients for potential academic, psychological and personal difficulties that may accompany a craniofacial condition. Our specialists can offer supportive therapy and provide guidance in dealing with peers and relatives, as well as make appropriate referrals for comprehensive evaluation and intervention.
Reviewed by Jesse A. Taylor, MD, Shelly Soni, MD




