Be Alert for Mood, Cognition Changes In Patients Newly Diagnosed with SLE
Published on
Children's DoctorPublished on
Children's DoctorA 15-year-old girl presented to her pediatrician with a 2-month history of rash and joint pain. During summer vacation she developed facial rash. Initially, it was thought to be sunburn, but it persisted. Her joints felt stiff and achy. On physical exam, she had a malar rash and a painless ulcer on her hard palate. She had effusions of wrists. The rest of her physical exam was normal. Labs revealed leukopenia, an elevated ESR, and low C3 and C4. Urinalysis and CMP were normal. She had a positive ANA of 1:1280 with a positive double-stranded DNA antibody. She was referred to Rheumatology and diagnosed with systemic lupus erythematosus. She was started on immunosuppressive therapy.
She initially does well and starts 10th grade, but then presents to her pediatrician 2 months later with difficulty concentrating and depressed mood. Her parents initially attribute her symptoms to stress from her new diagnosis and a demanding school workload. Normally an honor roll student, she is finding it difficult to focus on her work and her grades are falling. She seems sad and irritable. She is not interested in doing things with her friends. She admits to sometimes feeling suicidal and to hearing voices telling her to harm herself.
Discussion: The diagnosis is neuropsychiatric systemic lupus erythematosus (NPSLE). Systemic lupus erythematosus (SLE) is a chronic and episodic autoimmune vasculitis affecting multiple organs. It is rare, with an incidence of approximately 2 in 100,000 children, and typical onset in adolescent females. Neuropsychiatric manifestations of SLE occur in 20% to 95% of children with SLE and are associated with significant morbidity and mortality due to central nervous system damage.
Due to the heterogeneity of NPSLE manifestations, a high index of suspicion is needed for timely diagnosis. There are 19 NPSLE syndromes involving the central and peripheral nervous system; multiple syndromes can occur in an individual patient. The most common central nervous system syndrome in children is headache, followed by psychosis, cognitive dysfunction, cerebrovascular disease, seizures, mood and anxiety disorders, and chorea. Peripheral nervous system syndromes such as Guillain-Barre syndrome and mono- and polyneuropathies occur less commonly in children with SLE.
NPSLE can present prior to, concurrently with, or after presentation with other features of SLE. About 40% of pediatric-onset SLE patients present with neuropsychiatric features at initial SLE diagnosis, and 70% present within 1 year after diagnosis. However, 30% may present with neuropsychiatric features as late as 10 years after diagnosis. Thus it is important to keep in mind the possibility of NPSLE even after a diagnosis of SLE is made and immunosuppressive treatment is initiated.
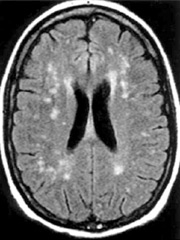 Figure 1: Brain MRI with contrast showing nonspecific foci of increased signal in the white matter of the frontal and parietal lobes.
Current diagnostic modalities for NPSLE rely on a combination of blood tests, cerebrospinal fluid analysis, conventional MRI, EEG, electrophysiology, neurocognitive testing, and subspecialty evaluation. Evaluation of blood tests for SLE disease activity and antiphospholipid antibodies is essential. Cerebrospinal fluid analysis typically shows elevated white cells and protein levels, and infection must be ruled out. MRI findings may include nonspecific foci of enhancement in the white and grey matter (see Figure 1), hemorrhage, infarct, pseudotumor cerebri, and cerebral atrophy. EEG and electrophysiology aid in detecting seizure activity and peripheral nervous system disease, respectively. Neurocognitive testing can detect impairments in attention, memory, visual-spatial processing, language, reasoning, psychomotor speed, and executive function. Psychiatric evaluation confirms hallucinations, delusions, and mood and anxiety disorders. Neurologist expertise is valuable for comprehensive neurological exam and assessment of neuroimaging.
Figure 1: Brain MRI with contrast showing nonspecific foci of increased signal in the white matter of the frontal and parietal lobes.
Current diagnostic modalities for NPSLE rely on a combination of blood tests, cerebrospinal fluid analysis, conventional MRI, EEG, electrophysiology, neurocognitive testing, and subspecialty evaluation. Evaluation of blood tests for SLE disease activity and antiphospholipid antibodies is essential. Cerebrospinal fluid analysis typically shows elevated white cells and protein levels, and infection must be ruled out. MRI findings may include nonspecific foci of enhancement in the white and grey matter (see Figure 1), hemorrhage, infarct, pseudotumor cerebri, and cerebral atrophy. EEG and electrophysiology aid in detecting seizure activity and peripheral nervous system disease, respectively. Neurocognitive testing can detect impairments in attention, memory, visual-spatial processing, language, reasoning, psychomotor speed, and executive function. Psychiatric evaluation confirms hallucinations, delusions, and mood and anxiety disorders. Neurologist expertise is valuable for comprehensive neurological exam and assessment of neuroimaging.
Despite these diagnostic resources, however, diagnosis of NPSLE is often challenging and complex due to limitations in definitively detecting SLE-related pathology and relies on cumulative information.
Similarly, management of NPSLE requires a multidisciplinary approach, including rheumatologists, neurologists, hematologists, psychologists, and psychiatrists. Immunosuppressive treatment is determined by the severity of NPSLE. Therapy aims to acutely control inflammation with glucocorticoids and effect long-term disease control with steroid-sparing immunosuppressive agents. Limiting glucocorticoid exposure is of high importance due to multiple adverse effects and possible steroid-induced psychosis. Anti-epileptics and neuropathic pain medications may be required. Anticoagulation is indicated for patients with evidence of antiphospholipid syndrome or other thrombotic state. Psychotropic medications and psychotherapy is indicated for psychiatric manifestations of NPSLE.
Although outcomes of children with NPSLE are generally favorable, neuropsychiatric disease remains a major source of morbidity and mortality for children with SLE. Approximately 80% of children with NPSLE respond to treatment with 60% achieving remission on minimal glucocorticoid. However, 20% of children with NPSLE will experience a relapse. Permanent central nervous system damage, such as persistent cognitive dysfunction, occurs in about 25%; those with seizures, cerebrovascular disease, recurrent central nervous system flares, and overall high SLE disease activity are at highest risk. Mortality due to NPSLE occurs in 5% to 30% of affected children. This underscores the importance of timely treatment and appropriate interdisciplinary management to achieve the best outcomes.
Our patient had a brain MRI showing nonspecific white matter foci and cerebral atrophy. Lumbar puncture showed a mild leukocytosis and elevated protein level. Blood tests were unremarkable. Neurocognitive testing showed impairment in attention, memory, and executive function. Her immunosuppressive therapy was intensified, and she was started on psychotropic medication with resolution of her neuropsychiatric symptoms.
Benseler SM, Silverman ED. Neuropsychiatric involvement in pediatric systemic lupus erythematosus. Lupus. 2007;16(8):564-571.
The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. ACR Ad Hoc Committee on Neuropsychiatric Lupus Syndromes. Arthritis Rheum. 1999;42(4):599-608.
Lim LS, Lefebvre A, Benseler S, Peralta M, Silverman ED. Psychiatric illness of systemic lupus erythematosus in childhood: spectrum of clinically important manifestations. J Rheumatol. 2013;40(4):506-512.
Yu HH, Lee JH, Wang LC, Yang YH, Chiang BL. Neuropsychiatric manifestations in pediatric systemic lupus erythematosus: a 20-year study. Lupus. 2006;15(10):651-657.
Jennings JE, Sundgren PC, Attwood J, et al. Value of MRI of the brain in patients with systemic lupus erythematosus and neurologic disturbance. Neuroradiology. 2004;46(1):15-21.
Categories: Rheumatology, Children's Doctor Winter 2016