When Diet and Exercise Aren't Enough
Published on
Children's DoctorPublished on
Children's DoctorJoy P. Collins, MD, and Elizabeth Prout, MD
Kaitlyn is a 17-year-old girl with severe obesity who presents to the Healthy Weight Clinic for weight management. Her mother describes her as having been a thin child until the age of 7, when she developed pubic hair and began to gain excessive weight. Kaitlyn was diagnosed with Kallman syndrome at the age of 11, which does not allow her to have a period without medical intervention. She has been followed by Endocrinology for Kallman syndrome.
Kaitlyn has continued to gain weight despite multiple weight loss attempts—both medically supervised and unsupervised—and currently has a body mass index (BMI) of 41 kg/m2. As her weight has increased, she has developed insulin resistance, acanthosis nigricans, hypertriglyceridemia, and non-alcoholic fatty liver disease. Acanthosis nigricans is either a darkening or thickening of skin found around the neck and under the armpits that signifies the insulin is having to work harder to control blood sugar and, along with insulin resistance, is a precursor to type 2 diabetes. Insulin resistance, fatty liver disease, and high triglycerides are all a part of metabolic syndrome.
Kaitlyn and her family were interested in weight loss surgery. The next step for her was to undergo a minimum of 6 months of weight management with our multidisciplinary Healthy Weight Program team. Given her severe obesity, we recommended a weight loss goal of between 1 to 2 lbs per week with a pre-surgical weight loss goal of 10% of her body weight. To treat her hypertriglyceridemia, we recommended a significant reduction of simple sugars in her diet and increased consumption of foods high in fiber and whole grains. For both the elevated triglycerides and fatty liver disease, we recommended a fructose-restricted diet, as fructose converts to fat and triglycerides in the liver. This meant limiting sugar-sweetened beverages and foods with high fructose corn syrup and sugar.
Kaitlyn met with our dietitian, who counseled her on these specific issues as well as on reducing portions and lowering her overall calories. Additionally, we recommended 45 to 60 minutes of moderately vigorous physical activity at least 5 days per week. She met with our physical activity specialist, who created a custom exercise program involving walking and resistance band training. She was also followed by our psychologist, who monitored her depression and self-esteem issues. The patient was very motivated and followed through on our recommendations. However, after 3 months of weight management, it was clear that she would not be able to achieve significant durable weight loss through lifestyle changes alone. Given the severity of her co-morbidities and her family history, we recommended weight loss surgery and began directive weight management to prepare Kaitlyn and her family for laparoscopic sleeve gastrectomy and life after surgery. Of note, the patient’s mother has previously had a Roux-en-y gastric bypass surgery with a subsequent sustained weight loss of 135 lbs over the past 10 years, and both parents were supportive throughout her weight management endeavors.
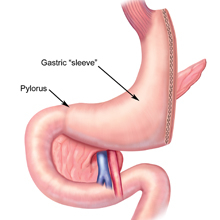 Because the laparoscopic sleeve gastrectomy (see Figure 1) has less surgical risk and fewer nutritional and medical complications than gastric bypass, this was the procedure recommended for our patient. Kaitlyn continued to meet with the Healthy Weight team and focused on monitoring her daily protein, not eating and drinking at the same time, eating 3 meals a day, drinking 64 oz of fluids, continuing to eat fiber, avoiding carbonated and sugar-sweetened beverages, and avoiding foods high in fat and sugar.
Because the laparoscopic sleeve gastrectomy (see Figure 1) has less surgical risk and fewer nutritional and medical complications than gastric bypass, this was the procedure recommended for our patient. Kaitlyn continued to meet with the Healthy Weight team and focused on monitoring her daily protein, not eating and drinking at the same time, eating 3 meals a day, drinking 64 oz of fluids, continuing to eat fiber, avoiding carbonated and sugar-sweetened beverages, and avoiding foods high in fat and sugar.
(Figure 1 Adapted from Atlas of Metabolic and Weight Loss Surgery published by Cine-Med Publishing, Inc., 2010, www.cine-med.com)
Her family had challenges of parental illness and financial difficulties, which led to missed appointments and prolonged her surgical preparation time. These issues were resolved, however, and Kaitlyn subsequently underwent the sleeve gastrectomy procedure. Her post-operative course was uneventful, and as of 6 months after surgery, she has lost a total of 85 lbs. She continues to exercise and consumes a high-protein, low-sugar/low-fat diet. She has normal liver function tests, no evidence of hypercholesterolemia, and an abundance of energy and self-confidence.
To refer a patient to the Healthy Weight Program or learn more about bariatric surgery for adolescents, call 267-426-2782.
McGuire MM, Nadler EP, Qureshi FG. Laparoscopic vertical sleeve gastrectomy for adolescents with morbid obesity. Semin Pediatr Surg. 2014;23(1):21-23.
Michalsky MP, Inge TH, Teich S, Eneli I, et al. Adolescent bariatric surgery program characteristics: the Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study experience. Semin Pediatr Surg. 2014;23(1):5-10.
Contributed by: Elizabeth Parks Prout, MD, MSCE
Categories: Surgery, Children's Doctor Winter 2015