The Power of Advanced Bronchoscopy: Fewer Surgeries, Impressive Results
Published on
Published on
By Joseph Piccione, DO, MS, and Pelton Phinizy, MD
When we first created a specific center to focus on emerging bronchoscopy techniques for children, our goal was to spare children unnecessary surgeries to diagnose pulmonary conditions such as pulmonary nodules, endobronchial tumors, enlarged lymph nodes in the chest, tumors of lung/mediastinum, lung infections, rare diffuse lung diseases and other pulmonary lesions.
With a more precise diagnosis, we could recommend more precise treatments, which is particularly critical for infections and certain tumors. Adults had enjoyed these options for years; it was time to bring these advances to the pediatric population.
Now, eight years since we began, we have expanded the services of the Pulmonary Advanced Diagnostic and Interventional Bronchoscopy Center at Children’s Hospital of Philadelphia (CHOP) to encompass minimally invasive treatment techniques for many conditions. Our team now performs cutting-edge procedures designed to treat narrowing of the tracheobronchial tree, persistent pneumothorax (also called “persistent air leak”), tracheoesophageal fistula, pulmonary alveolar proteinosis (PAP) and difficult-to-remove foreign bodies.
These less invasive methods for diagnosis and treatment reduce children's risk of complications, discomfort and overnight hospital stays.
We recently published an article in Pediatric Pulmonology that quantified diagnostic outcomes as a resounding success.
Minimally invasive techniques for transbronchial lung and lymph node biopsies under endobronchial ultrasound (EBUS) or computerized tomography (CT) guidance provide a way to gather samples of lung and lymph node tissue without surgical biopsy. CHOP began performing EBUS-guided transbronchial lung and lymph node biopsies in 2015. There are two forms of EBUS advanced techniques:
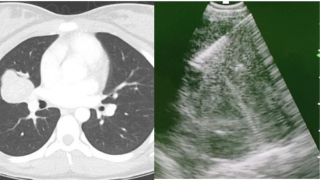 (L) CT scan image of enlarged lymph node; (R) Linear endobronchial ultrasound image of needle inside the lymph node
1. Linear EBUS transbronchial needle aspiration is used to sample mediastinal, tracheal and bronchial lymph nodes or lesions. This technique can be helpful in diagnosing conditions such as sarcoidosis, sarcoma, lymphoma, carcinoma and tuberculosis. Children with histoplasmosis, lymphoma, metastatic tumors and sarcoidosis have been successfully and safely diagnosed with EBUS-guided transbronchial lymph node aspiration techniques at CHOP.
(L) CT scan image of enlarged lymph node; (R) Linear endobronchial ultrasound image of needle inside the lymph node
1. Linear EBUS transbronchial needle aspiration is used to sample mediastinal, tracheal and bronchial lymph nodes or lesions. This technique can be helpful in diagnosing conditions such as sarcoidosis, sarcoma, lymphoma, carcinoma and tuberculosis. Children with histoplasmosis, lymphoma, metastatic tumors and sarcoidosis have been successfully and safely diagnosed with EBUS-guided transbronchial lymph node aspiration techniques at CHOP.
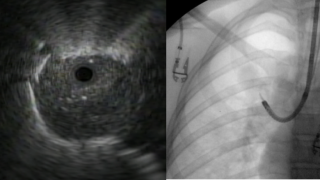 (L) Radial endobronchial ultrasound image of peripheral lung lesion; (R) Chest X-ray image of radial ultrasound probe extending out of the bronchoscope
2. Radial EBUS is helpful in identifying the cause of peripheral pulmonary nodules. The radial EBUS probe allows us to locate the peripheral lesions and obtain biopsies with greater accuracy. Radial EBUS is often combined with CT navigation to guide the bronchoscope to the location of the peripheral lesion. Immunocompromised children with pneumonia may benefit from EBUS-guided transbronchial lung biopsy, which can identify the specific infection present so treatment can be targeted.
(L) Radial endobronchial ultrasound image of peripheral lung lesion; (R) Chest X-ray image of radial ultrasound probe extending out of the bronchoscope
2. Radial EBUS is helpful in identifying the cause of peripheral pulmonary nodules. The radial EBUS probe allows us to locate the peripheral lesions and obtain biopsies with greater accuracy. Radial EBUS is often combined with CT navigation to guide the bronchoscope to the location of the peripheral lesion. Immunocompromised children with pneumonia may benefit from EBUS-guided transbronchial lung biopsy, which can identify the specific infection present so treatment can be targeted.
3. CT navigational bronchoscopy uses CT imaging to create a road map to the pulmonary lesion. This technique is frequently used in conjunction with endobronchial ultrasound and improve our ability to locate pulmonary lesions requiring lung biopsy more precisely.
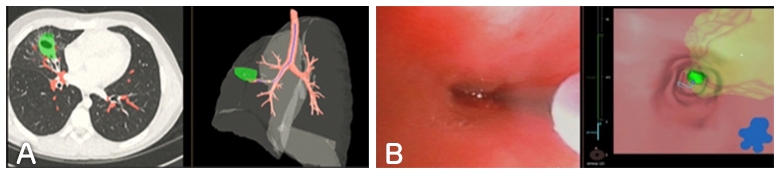
Figure A: CT image and superimposed virtual navigation pathway and target lesion (green sphere) Figure B: Bronchoscopic image alongside virtual bronchoscopic image alongside with target lesion (green sphere) and virtual pathway (blue line)
Advances in flexible bronchoscopy technology now allow for minimally invasive procedures to relieve obstruction in the airway due to tumors, plastic bronchitis, bronchial casts, blood clots and inhaled foreign bodies. These advances have also provided alternatives to surgery for some children with tracheoesophageal fistula, pneumothorax and hyperinflated/emphysematous lung.
Some specific interventions include:
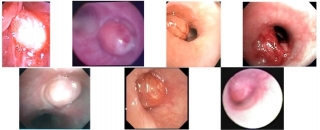 Airway tumors as seen through bronchoscopy
Airway tumors as seen through bronchoscopy
1. Diagnosis and treatment of tracheal and bronchial tumors
While rare, tumors and masses of the trachea and bronchi do exist in children. At CHOP, we pull together specialists in pulmonology, otolaryngology, oncology, radiology, pathology and cardiothoracic surgery to treat these patients. Flexible and rigid bronchoscopy techniques allow for biopsy to determine the cause of the mass and to differentiate between true tumors and those caused by infections or inflammatory conditions. This information has a major impact on treatment.
The most common types of airway tumors in children are carcinoid tumors, inflammatory myofibroblastic tumors and mucoepidermoid carcinomas. Sometimes, complete removal of certain types of tumors is possible using flexible and/or rigid bronchoscopy.
2. Cryosurgical and cryoextraction bronchoscopy
Cryotherapy is a technique that uses rapid development of freezing temperatures. This technology has been adapted for use in flexible bronchoscopy and provides effective ways to remove foreign bodies, mucus plugs, blood clots and bronchial casts caused by plastic bronchitis from the airways in children (cryoextraction). These tools are increasingly becoming the preferred approach, replacing historically standard instruments (e.g., suction, forceps, baskets). Cryotherapy approaches can also be used to treat bronchial narrowing/stenosis (cryodevitalization) and to obtain tissue samples (cryobiopsy).
3. Balloon dilation for bronchial stenosis
Congenital or acquired bronchial stenosis may be treated with specially designed balloon catheters that stretch and expand the airway. This is sometimes used together with cryotechnology to freeze the scar and prevent it from returning.
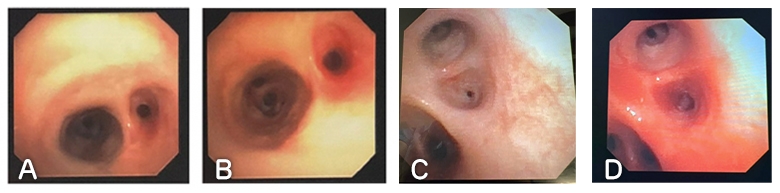
Figure A: the view of the right upper lobe (RUL) bronchus that was obstructed with circumferential stenosis. Figure B: the area after balloon dilation. Figure C: Circumferential stenosis of a segmental bronchus before balloon dilation. Figure D: the same bronchus after balloon dilation.
4. Endobronchial valves
 Endobronchial valve in an airway
Endobronchial one-way valves were developed as nonsurgical alternatives to lung volume reduction surgery in adults with COPD (chronic obstructive pulmonary disease)/emphysema and lung collapse requiring a chest tube due to persistent air leak (pneumothorax). Endobronchial valves have been used in select cases for infants and children with pneumothorax.
Endobronchial valve in an airway
Endobronchial one-way valves were developed as nonsurgical alternatives to lung volume reduction surgery in adults with COPD (chronic obstructive pulmonary disease)/emphysema and lung collapse requiring a chest tube due to persistent air leak (pneumothorax). Endobronchial valves have been used in select cases for infants and children with pneumothorax.
5. Nonsurgical treatment of tracheoesophageal fistula
Congenital or acquired tracheoesophageal fistulas (TEF) are another condition ripe for noninvasive treatment. Most children with tracheoesophageal fistulas are also born with esophageal atresia. Typically, surgery is performed to repair the fistula early in life. However, TEF can be found in isolation (without esophageal atresia), can recur after initial surgical repair, or multiple TEF can exist in the same child and may not always be found at the early surgeries. For these children, techniques have been developed to identify and locate persistent or recurrent fistula and to close the fistula using a combination of bronchoscopy and endoscopy instead of surgery.
Instruments can be inserted into the flexible bronchoscope and endoscope to carefully and precisely deliver an electrical current that causes the hole to scar closed. Specially designed clips can also be used to help keep the hole closed. Pulmonary specialists from the Advanced Diagnostic and Interventional Bronchoscopy Center have partnered with experts in gastroenterology, ENT and pediatric surgery to offer endoscopic TEF repair through the Esophageal and Airway Treatment Program.
We’re excited about the strides we’ve made in adapting noninvasive bronchoscopy techniques for children. Even with these advances, we are unwavering in our commitment to advance and develop new ways to diagnose lung disease in children and our center will add additional techniques as they become available. If you have a patient who would benefit from our experience with minimally invasive pulmonary diagnostic and treatment methods, please reach out to discuss how we may be able to spare the child from surgery. Contact us:
See additional information about our Pulmonary Advanced Diagnostic and Interventional Bronchoscopy Center.