Gastroesophageal Reflux Disease (GERD)
What is gastroesophageal reflux (GER)?
Gastroesophageal reflux (also called GER) is a digestive disorder.
Gastroesophageal refers to the stomach and esophagus. Reflux means to flow back or return. Gastroesophageal reflux is the return of acidic stomach juices, or food and fluids, back up into the esophagus.
When does GER become GERD?
When a baby has reflux that results in other health issues or concerns and requires further treatment, it is often called gastroesophageal reflux disease (GERD).
It is important to understand the difference between GER and GERD. Gastroesophageal reflux is common in babies, although it can occur at any age. It is often a temporary condition. GERD, on the other hand, may become a long-term physical problem.
What causes GER?
Gastroesophageal reflux is often the result of conditions that affect the lower esophageal sphincter (LES). The LES, a muscle located at the bottom of the esophagus, opens to let food into the stomach and closes to keep food in the stomach. When this muscle relaxes too often or for too long, acid refluxes back into the esophagus, causing nausea, vomiting or heartburn.
As infants digest their feedings, the LES may open and allow the stomach contents to go back up into the esophagus. Sometimes, the stomach contents go all the way up the esophagus and the baby vomits. Other times, the stomach contents only go part of the way up the esophagus, causing heartburn, breathing problems, or, possibly, no symptoms at all.
It is important to understand the difference between GER and GERD. GERD refers to gastroesophageal reflux disease. GERD occurs when a baby has reflux that results in other health issues or concerns and often requires further treatment.
Why is GERD a concern?
Most babies with GER have no symptoms other than frequently spitting up. As long as these babies are growing well and not developing other health problems associated with GERD, such as breathing difficulties, the condition needs no treatment and will resolve on its own with time.
Babies with GERD who vomit frequently may not gain weight and grow normally. Inflammation (esophagitis) or ulcers (sores) can form in the esophagus due to contact with stomach acid. These ulcers can become painful and also may bleed, leading to anemia (too few red blood cells in the bloodstream). Esophageal narrowing (stricture) and Barrett's esophagus (abnormal cells in the esophageal lining) are long-term complications from inflammation that typically occur in adults.
Some babies who have GERD may not vomit, but may still have stomach contents move up the esophagus and spill over into the windpipe (the trachea). This can cause wheezing, pneumonia, poor weight gain, and in very rare cases, a possibly life-threatening event.
What are the symptoms of GERD?
The following are other common symptoms of GERD. However, each baby may experience symptoms differently. Symptoms may include:
- Belching
- Refusal to eat
- Stomachache
- Fussiness around mealtimes
- Arching of the back when lying flat
- Hiccups
- Gagging
- Choking
- Frequent cough
- Coughing fits at night
- Wheezing
- Frequent ear infections
- Rattling in the chest
The symptoms of GERD may resemble other conditions or medical problems. Always consult your baby's doctor for a diagnosis.
How is GERD diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures that may be performed to help evaluate gastroesophageal reflux include:
- Chest X-ray. A diagnostic test to look for evidence of aspiration a condition in which stomach contents spill into the lungs leading to breathing problems and lung infections.
- Upper GI (gastrointestinal) series. A diagnostic test that examines the organs of the upper part of the digestive system: the esophagus, stomach and duodenum (the first section of the small intestine). A fluid called barium, a metallic, liquid used to coat the inside of organs so that they will show up on an X-ray, is swallowed. X-rays are then taken to evaluate the digestive organs.
- Endoscopy. A test that uses a small, flexible tube with a light and a camera lens at the end (endoscope) to examine the inside of part of the digestive tract. Tissue samples from inside the digestive tract may also be taken for examination and testing.
- pH testing. A measurement of the level of acidity in the esophagus.
- Gastric emptying studies. A test designed to determine whether or not the stomach contents empty into the small intestine properly. Delayed gastric emptying can contribute to GERD, allowing stomach contents to back up into the esophagus.
What is the treatment for GERD?
Specific treatment for gastroesophageal reflux will be determined by your baby's doctor based on:
- Your baby's gestational age, overall health, and medical history
- The extent of the disease
- Your baby's tolerance for specific medications, procedures or therapies
- The expectations for the course of the disease
- Your opinion or preference
Feeding/dietary treatment
In many cases, GERD can be relieved through feeding changes, under the direction of your baby's doctor. Some ways to better manage GERD symptoms include the following:
- After feedings, hold your baby in an upright position for 30 minutes. Stomach sleeping has been associated with an increased risk for Sudden Infant Death Syndrome (SIDS), check with your baby's doctor about how to position your baby for sleeping.
- If bottle-feeding, keep the nipple filled with milk so your infant does not swallow too much air while eating. Try different nipples to find one that allows your baby's mouth to make a good seal with the nipple during feeding.
- Adding rice cereal to feeding may be beneficial for some older babies.
- Burp your baby several times during bottle-feeding or breastfeeding. Your baby may reflux more often when burping with a full stomach.
- Make sure your baby's diaper is not too tight since this can exacerbate reflux.
Medical treatment
Treatment may include:
- Medications. If needed, your baby's doctor may prescribe medications to help with reflux. There are medications that help decrease the amount of acid the stomach makes, which, in turn, will cut down on the heartburn associated with reflux. Other medications can help the stomach to empty more quickly.
- Calorie supplements. Some babies with reflux will not be able to gain weight due to frequent vomiting. Your baby's doctor may recommend:
- Providing your infant with more calories by adding a prescribed supplement to formula or breast milk to make the milk higher in calories than normal.
- Change formula to milk-free or soy-free formula if signs of allergy present that are not seen with breast milk. Symptoms may include rash, history of milk sensitivity in the family, constipation or diarrhea.
- Tube feedings. Some babies with reflux have other conditions that make them tired, such as congenital heart disease or prematurity. In addition to having reflux, these babies may not be able to drink very much without becoming sleepy. Other babies are not able to tolerate a normal amount of formula in the stomach without vomiting, and would do better if a small amount of milk was given continuously. In both of these cases, tube feedings may be recommended. Formula or breast milk is given through a tube that is placed in the nose, guided through the esophagus, and into the stomach (nasogastric tube). Nasogastric tube feedings can be given in addition to, or instead of, what a baby takes from a bottle. Nasoduodenal tubes can also be used to bypass stomach.
Many babies with GERD will "outgrow it" by the time they are about a year old, as the lower esophageal sphincter becomes stronger. For others, medications, lifestyle and dietary changes can minimize reflux, vomiting and heartburn.
Surgical treatment for gastroesophageal reflux disease (GERD): Fundoplication
If gastroesophageal reflux is more severe and long-lasting and causing other health issues, it may be diagnosed as gastroesophageal reflux disease (GERD).
Anti-reflux surgery is a treatment option when reflux cannot be managed with medications and results in problems such as poor weight gain, breathing problems, aspiration (stomach contents entering the lungs), chronic ear infections, or apnea spells.
The purpose of surgical intervention for GERD is to improve health and growth by relieving the symptoms that reflux causes. GERD surgery is generally a very effective treatment option, with more than 90% of patients gaining control of reflux after the procedure.
The surgical procedure used to treat GERD is called a fundoplication.
Types of fundoplication surgery
The purpose of a fundoplication is to restore the anatomic and physical function of the valve complex so there is low resistance for food going down, but high resistance against food coming up. Surgery is used to reinforce the lower esophageal sphincter and mechanically discourage reflux.
There are several types of anti-reflux surgery procedures (also called a fundoplication) that may be used. These include:
- Nissen fundoplication (also called a floppy Nissen)
- Toupet fundoplication
- Thal fundoplication
Each approach is similar, and involves wrapping a portion of the stomach around the esophagus to prevent reflux. The difference between the three procedures is how far the stomach is wrapped around the esophagus. The decision of which procedure to use is based on every child’s unique condition, and will be discussed prior to surgery.
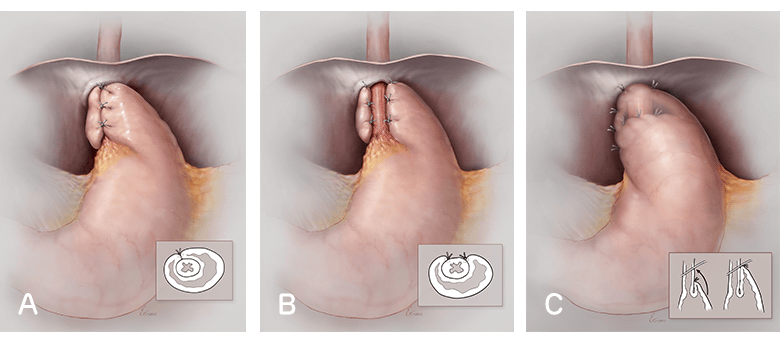
(A) In a Nissen fundoplication, the surgeon wraps the top of the stomach around the lower esophagus 360-degrees, creating a loose, short wrap. (B) In a Toupet fundoplication, the surgeon wraps the stomach partially around the back of the esophagus for a 270-degree wrap, creating an anti-reflux valve which grows with the patient. (C) In a Thal fundoplication, the surgeon partially wraps the stomach around the front part of the esophagus.
Preparing for GERD surgery
Prior to your child’s surgery, you will have a preoperative visit with your surgical team.
During the pre-visit, we'll discuss individual anesthesia needs and pain management strategies, provide detailed preoperative feeding/drinking instructions, and an overview of what to expect on the day of surgery. Our surgical advanced practice nurses will provide age-appropriate preparation for your child’s procedure.
You can expect to stay in the hospital overnight or for a few nights while your child recovers.
Learn more about what to expect before, during and after surgery at CHOP.
What to expect after GERD surgery
After surgery, your child will be admitted for a short hospital stay, during which we will monitor for any complications and make sure they are able to tolerate feedings well before they are sent home.
After an anti-reflux procedure, in rare cases some children may experience post-prandial hypoglycemia (sometimes called “dumping”). This means that children and babies will sometimes have a very high then dangerously low blood glucose level (hypoglycemia) after a feeding. We will screen for this postoperatively while your child is in the hospital. If your child experiences this, we will change their feeding regimen while you’re in the hospital and discharge your child once the hypoglycemia is resolved.
Gagging or retching may occur postoperatively, which can be managed by “venting” the g-tube or adjustments of feeds. Retching is usually not a sign of untreated reflux! Instead, retching is frustrated vomiting. Anything that might provoke vomiting can produce retching in a child after fundoplication.
Some children may experience difficulty or discomfort with swallowing (dysphagia) after surgery. If your child is taking food by mouth, a soft, slippery diet is recommended for a period of time. Your child’s surgical team and dietitians will work with your family to manage their feedings and make sure they are well-tolerated before discharge.
Why choose CHOP for GERD surgery?
CHOP’s pediatric surgeons and advanced practice providers take an individualized approach to determine the best surgical approach for each child.
Our team has extensive experience performing all the different laparoscopic anti-reflux surgery procedures that may benefit your child. We see these cases often and are comfortable using all techniques. This allows us to customize each child’s repair, accounting for any unusual anatomy or physiology.
CHOP’s board certified pediatric anesthesiologists are experts in keeping children comfortable and safe before, during and after any surgical procedure.
Your child will also have access to built-in dietitian support and any other subspecialists they may need to manage their care both after surgery and long-term.



























