Fetal Pleural Effusion
What is fetal pleural effusion?
Fetal pleural effusion is an accumulation of fluid in the chest cavity of a developing fetus. As the fluid increases, it can compress the developing lungs and heart. The underlying cause of pleural effusion in a fetus may include genetic issues, infection, and heart or lung conditions.
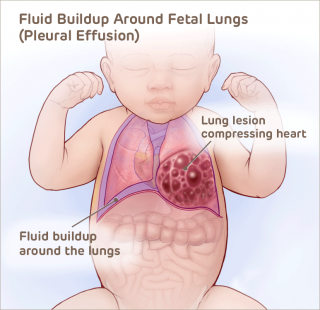 The outlook for each individual case depends on the amount of fluid in the chest. A high amount of fluid can lead to fetal heart failure (hydrops) and pulmonary hypoplasia (underdeveloped lungs).
The outlook for each individual case depends on the amount of fluid in the chest. A high amount of fluid can lead to fetal heart failure (hydrops) and pulmonary hypoplasia (underdeveloped lungs).
Fetal pleural effusion is sometimes also called fetal hydrothorax.
Evaluation and diagnosis of fetal pleural effusion
A pleural effusion typically presents before the 32nd week of pregnancy. A diagnosis of pleural effusion is usually made by ultrasound. Families referred to the Center for Fetal Diagnosis and Treatment (CFDT) undergo a comprehensive one-day evaluation that may include the following studies:
- High-resolution fetal ultrasound — comprehensive imaging used to confirm the diagnosis and the severity of organ compression. This exceptionally detailed exam gives us a thorough view of the fetal anatomy, as well as analysis of the overall fetal growth and development.
- Fetal echocardiogram — a specialized ultrasound evaluation of the fetal heart, performed by fetal cardiologists, to assess structure and function.
- Ultrafast fetal MRI — an imaging technique pioneered at Children's Hospital of Philadelphia (CHOP) that can be useful in evaluating the chest organs in more complex cases.
- Fetal chromosome studies (karyotype) — laboratory studies to rule out chromosomal abnormalities that would affect the baby’s survival or long-term outcome.
A thorough prenatal evaluation will determine whether or not your baby may benefit from fetal intervention. After your evaluation is complete, our multidisciplinary team meets with your family to review imaging and test results, discuss the diagnosis, explain treatment options and potential outcomes, and answer any questions you may have.
Treatment for fetal pleural effusion
Depending on the diagnosis, fetal intervention may be an option for treating pleural effusion.
Thoracentesis (fluid drainage)
If fluid accumulates in the fetal chest and is severely compressing the fetal heart and lungs, we can perform a thoracentesis, a procedure performed under continuous ultrasound guidance in which we use a small needle to drain the fluid.
Austin's Story
Draining the fluid relieves the pressure on the baby’s heart and lungs. The fluid will be tested to determine its origin – this helps us identify the cause of the fluid buildup and guide treatment. The fluid is also tested for infection and chromosomal abnormalities.
In some cases the fluid may reaccumulate 24 to 72 hours after the procedure. If this occurs, a thoracoamniotic shunt can be placed for continuous fluid drainage.
Fetal thoracoamniotic shunt
A shunt is a hollow tube that provides a passageway for the excess fluid to go from the fetal chest cavity through the chest wall to the amniotic fluid space around the fetus. The mother receives antibiotics and IV sedation (which also sedates the baby).
Under ultrasound guidance and color-flow Doppler, a large trocar (hollow needle) is guided through the mother’s abdomen and uterus and then inserted through the fetus’s chest wall to remain in place until delivery.
After the procedure, expectant mothers receive antibiotics and are monitored for any post-procedural complications. You will be discharged the same day of shunt placement and return to CHOP one week later to ensure the shunt is functioning properly. After post-procedural follow-up, mothers who have undergone prenatal surgery return home and are monitored by their local care team.
Effective fluid drainage via thoracentesis or thoracoamniotic shunt placement leads to a decrease in fluid volume. This helps to improve lung growth, resolves hydrops, and improves long-term survival rates.
Delivery of babies with fetal pleural effusion
Mothers carrying babies with fetal pleural effusion may be able to deliver at their local hospital, without the need for high-risk neonatal care. Babies with large effusions or associated disorders should be delivered in a center that offers expert care for both mother and baby in one location.
At CHOP, babies with prenatally diagnosed pleural effusion who will require treatment immediately or soon after birth are delivered in the Garbose Family Special Delivery Unit, specifically designed to keep mother and baby together and avoid transport of fragile infants.
Here, your baby has immediate access to the Newborn/Infant Intensive Care Unit (N/IICU) and a dedicated Neonatal Surgical Team. Our team is experienced in performing complex, delicate procedures, as babies born with pleural effusion may need chest tube placement for continued fluid drainage, as well as intubation and respiratory support.
In more complicated cases, minimally invasive treatment of lymphatic malformations within the chest and lung may be required, as well as supplemental oxygen for respiratory support at the time of discharge. CHOP’s Center for Lymphatics Imaging and Interventions provides highly specialized care for children with lymphatic leaks and lymphatic flow disorders.
The neonatal team will provide a thorough evaluation of your child's condition and counsel your family on what to expect in both the short- and long-term, and connect you with any other subspecialists your child may need to see.
Reviewed by N. Scott Adzick, MD, MMM, FACS, FAAP