Human Papillomavirus: The Disease & Vaccines
Human Papillomavirus: The Disease & Vaccines
prevent-hpv.org
Questions and Answers about HPV and the Vaccine
View a list of questions submitted by readers on our companion webpage at prevent-hpv.org.
The disease
What is human papillomavirus?
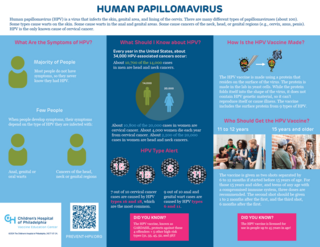
Human papillomavirus (HPV) is a virus that can infect the skin, genital and anal areas and lining of the cervix. There are many different types of papillomaviruses (about 100). Some types of papillomaviruses cause warts on the skin; some types cause warts in the anal and genital areas, and some types cause cervical cancer.
Many different HPV types cause cervical cancer. Two types (16 and 18) are the most common, accounting for about 7 of every 10 cases of cervical cancer. Similarly, many types of HPV cause anal and genital warts, but only two types (6 and 11) account for about 9 of every 10 cases.
The HPV vaccine, known as GARDASIL, protects against nine types of HPV that cause disease in people. The types in the vaccine are 6, 11, 16, 18, 31, 33, 45, 52, and 58.
Other viruses can cause cancer, too. For example, hepatitis B virus can cause liver cancer; AIDS virus can cause sarcoma (cancer of skin and soft tissues), and Epstein-Barr virus (the virus that causes 'mono') can cause cancers of the head and neck and of the immune system. These types of cancers can also be caused by other things. For example, alcohol can cause liver cancer; the sun can cause skin cancer, and poisons can cause cancer of the immune system.
Cervical cancer is unique in that almost all cases are caused by HPV. In some instances, HPV is not identified. Some of these cases are likely still caused by HPV, but the virus is not detected due to test sensitivity or inaccurate results. In other cases, the cancer could be misdiagnosed (i.e., metastasized or of a nearby tissue type) or a type of cancer, called adenocarcinoma, that is associated with local glands, rather than the squamous epithelial cells that line the cervix.

HPV video
HPV: Transmission, cancers & vaccination
Find out more about HPV in this video discussion between Drs. Paul Offit and Katie Lockwood.
How common is HPV?
HPV is the most common sexually transmitted disease in the United States and in the world. Twenty million Americans are currently infected with HPV and about 13 million Americans are infected every year. Half of those newly infected with HPV are between 15 and 24 years of age.
Is HPV dangerous?
Yes. Although most HPV infections typically resolve on their own, some persist. Every year in the United States:
- About 34,000 HPV-associated cancers occur:
- More than 20,000 of these are in females
- Almost 14,000 are in males
- The most common types of cancer caused by HPV infections are cervical cancer and head and neck cancers:
- About 10,800 cases of cervical cancer and 4,000 deaths occur annually
- About 10,700 males and 2,200 females are diagnosed with cancers of the head and neck
- Babies can also be infected when they pass through the birth canal of a mother infected with HPV. Some of these children go on to develop a long-term infection of their windpipe that is occasionally fatal. This disease is called recurrent respiratory papillomatosis.
How do you catch HPV?
HPV is transmitted from one person to another by genital contact. Although this most often occurs during sexual intercourse, it can also occur during oral or anal sex or through genital-to-genital contact in the absence of sexual intercourse.
HPV infections are unique. First, most people never know they were infected. Unlike a cold in which symptoms develop a few days after exposure to the virus, HPV infections are typically not symptomatic. Second, HPV infections can last for long periods of time. The average length of infection is about eight months; however, for about 1 of every 10 women, the infection lasts longer than two years. It is in this group of women that there is an increased risk of developing cervical cancer. Cervical cancer often doesn’t occur until 20 years after the initial infection.
How can you avoid getting HPV?
Sometimes people can be infected with HPV and not know it, so HPV can be difficult to avoid. The best way to avoid genital infection with HPV is abstinence. You can also decrease your chance of getting HPV by having sex with only one other person who isn't infected with HPV. While condoms may also decrease the chance of getting HPV, they do not always work to prevent the spread of the infection. Because other than abstinence, none of these measures can completely protect someone from becoming infected or prevent the spread of this infection, the development of a vaccine was an important tool for preventing future generations from experiencing the devastation caused by HPV.
Can't I avoid cervical cancer by simply getting routine Pap testing?
No. At one time cervical cancer was the most common cause of cancer in the United States. One test changed that: the Papanicolaou (Pap) test. The Pap test is performed by scraping cells from the opening of the cervix and examining them under the microscope to see whether they have begun to show changes consistent with the early development of cancer (called pre-cancerous changes). Typically, the length of time from infection with HPV to development of cervical cancer is about 15-20 years. For this reason, although most HPV infections occur in teenagers and young adults, cervical cancer is more common in women in their 40s and 50s.
The Pap test is one of the most effective cancer screening tests available and has dramatically reduced the incidence of cervical cancer in the United States. But the test isn't perfect and not all women get tested as often as they should.
On the flip side, even if you have been vaccinated against HPV, you are still recommended to get the Pap test.
Can genital HPV infections be treated?
HPV infections cannot be treated; however, the symptoms of HPV can be treated, at least to some extent. For example, genital warts can be treated with medications or surgically removed; however, they may return, and the patient may still be infected with HPV and could, therefore, still transmit the infection.
The vaccine
How is the HPV vaccine made?
The HPV vaccine is made using a protein that resides on the surface of the virus. The protein is grown in the lab in yeast cells. Once the protein is grown, it assembles itself to look like the HPV virus; however, importantly, it does not contain HPV genetic material, so it can’t reproduce itself or cause illness. The vaccine is composed of the surface protein from nine different types of HPV.
Who should get the HPV vaccine?
The Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics (AAP) recommend that all adolescents between 9 and 12 years of age receive the HPV vaccine.
The vaccine is given as two shots separated by 6 to 12 months if started before 15 years of age. For those 15 years and older, and teens of any age with a compromised immune system, three doses are recommended. The second shot should be given one to two months after the first, and the third shot, six months after the first. The HPV vaccine is licensed for use in people up to 45 years of age.
Learn more about why adolescents and teens are recommended to get HPV vaccine by watching this short video, part of the series Talking About Vaccines with Dr. Paul Offit.
Does the HPV vaccine work?
Yes. The HPV vaccine was originally studied in about 30,000 girls and young women between 9 and 26 years of age. Studies determined that the vaccine prevented 9 of 10 HPV infections and was completely effective at preventing persistent infections and Pap smear changes that predict cervical cancer. Subsequent studies showed that HPV vaccine prevented HPV infection, anal and genital warts, and anal cancer in men.
In Australia, where a school-based immunization program was implemented, they have seen dramatic reductions in pre-cancerous cervical changes in young women as well as genital warts in both young men and young women.
Is the HPV vaccine safe?
Yes. Because the HPV vaccine is made using only the surface protein from the virus, it can't cause HPV and, therefore, can't cause cervical cancer. The vaccine may cause redness and tenderness at the site of injection. The vaccine may also cause a low-grade fever in a small number of recipients. Fainting has been reported; however, the rates have not been higher than those following receipt of other vaccines for teens. Because of the possibility of fainting, teens are recommended to remain at the office for about 15-30 minutes after getting immunized.
More than 100 million doses of HPV vaccine have been given to people in the United States, and safety networks have continued to monitor reactions to the HPV vaccine since its licensure. Despite concerns raised by the media and some citizen groups, no cause-effect links have been found between HPV vaccine and adverse events, including blood clots, allergic reactions, strokes, seizures, Guillain-Barré Syndrome (GBS, a rare cause of paralysis), birth defects, miscarriages, infertility or premature ovarian failure, or infant/fetal deaths.
Studying vaccine safety
One example of a study that contributed understanding to HPV vaccine safety was a systematic review and meta-analysis. When scientists conduct this type of study, they systematically locate as many papers as they can about a particular topic and use criteria to evaluate the quality of each before using statistical analyses to evaluate and summarize what all of the studies together indicate about the issue, in this case what is known about the relationship between HPV vaccine and autoimmune diseases.
What is a systematic review?
Typically, during the systematic review, many papers are eliminated because they do not meet certain predetermined criteria, such as:
- They are not directly related to the topic at hand.
- They are not original research studies, but rather other types of papers, like case reports, which describe a finding without performing a controlled study, or an editorial, which, like in a newspaper, is a letter by someone with knowledge offering their thoughts.
- They are not peer-reviewed. Having other scientists review a study before it is published is an important part of the research process. Think of these people as the “officials in the booth” when a questionable play occurs on the football field. They know the rules, and they make a decision based on how well the rules were followed. The main difference, however, is that when it comes to scientific publications, virtually every paper gets reviewed by the booth, not just a few questionable plays. Journals that allow papers to be published without going through the peer review process may have sound scientific papers, but often, they have papers that could not make it past the reviewers.
What did these researchers learn about HPV vaccine safety?
Of the 541 papers located, 137 were considered close enough to the topic by virtue of their titles and abstracts that they were reviewed. Only 20 met all of the criteria for inclusion in the statistical part of the study. This may sound like a very small final number, but this shows how important it is to understand that just because a paper may seem like it is about a topic does not mean it is useful for answering a particular question. Also, of interest, of the 20 studies evaluated, five of them were determined to be of “low quality” based on their lack of scientific rigor.
During this particular review, researchers determined that the HPV vaccine did not cause increases in any of the following types of autoimmune disorders:
- Neurological — Disorders involving the brain or nervous system, including Bell’s palsy, epilepsy, Guillain-Barré syndrome, multiple sclerosis, narcolepsy, optic neuritis, or paralysis
- Gastrointestinal — Disorders involving the digestive tract, including inflammatory bowel disease, Crohn’s disease, ulcerative colitis, celiac disease, or autoimmune pancreatitis
- Musculoskeletal or systemic — Disorders including ankylosing spondylitis, rheumatoid or juvenile arthritis, systematic lupus erythematosus, or vasculitis
- Hematological — Disorders of the blood including autoimmune hemolytic anemia, Henoch-Schönlein purpura, and idiopathic thrombocytopenic purpura
- Dermatological — Disorders involving the skin, including scleroderma, psoriasis, and vitiligo
- Diabetes — type 1 diabetes
- Thyroid disorders — Grave’s disease, hypothyroidism, and hyperthyroidism did not correlate with receipt of HPV vaccine. On the other hand, data suggested Hashimoto’s thyroiditis may be correlated. The authors pointed out, however, that this finding was not likely to be an actual risk for a few reasons. First, the populations studied and the methodology used in the studies may have confounded the results. Second, all of the other thyroid-based diseases, including hypothyroidism, which is typically caused by Hashimoto’s thyroiditis, were negative.
Other questions you might have
To find answers to dozens of questions about HPV and the vaccine, check prevent-HPV.org.
Why do adolescents need the HPV vaccine?
The HPV vaccine is recommended before the start of sexual activity for two reasons:
- Young people tend to get infected more frequently. In fact, about half of all new infections are diagnosed in young people between 15 and 24 years of age.
- It takes six months to complete the series, so even though your son or daughter may not be active now, or even in six months, it is better to have the series completed sooner rather than later.
What HPV testing is available?
Men
HPV tests for men are not available, and most HPV infections clear on their own without causing problems. However, health problems caused by HPV, which can include genital warts, anal cancer, penile cancer or cancers of the head and neck, can be checked by visiting your doctor.
Women
Women can get HPV tests and/or Pap tests to determine whether they have an HPV infection that can lead to cervical cancer. Both tests detect early health problems that can lead to cervical cancer, but neither checks for warning signs of other cancers, fertility or other STDs. Although both tests have a common goal, they do have their differences:
Pap test (Pap Smear)
- Recommended for women 21 and older.
- Involves scraping the cervix to identify any abnormal changes in cells of the cervix that could later develop into cancer.
- Results are typically reported as “normal,” “unclear,” or “abnormal”:
- “Normal” means that no changes were found in the cells
- “Unclear” indicates that the cells look like they could be abnormal
- “Abnormal” means that changes in cervical cells were found
- If your Pap test comes back “normal,” you should still get Pap tests according to the recommended schedule to be sure new changes haven’t occurred.
- If your Pap test comes back “unclear” or “abnormal,” more testing will be required.
HPV test
- Most often recommended for women 30 and older and women 21 and older who have had an abnormal Pap test.
- Typically performed at the same time as a Pap test, using either the same sample as the Pap test or a second sample of cells scraped from the cervix.
- “Positive” results mean that your cervix has the types of HPV commonly linked to cervical cancer. “Negative” results mean that you do not have any types of HPV that are specifically linked to cervical cancer.
- Helps your doctor determine how frequently you should be tested and whether other tests should be performed.
If both tests are normal, it is highly unlikely that serious cervical cell changes will develop in the next three years; however, regular wellness visits should not be skipped.
If either test is abnormal, more testing will be completed. Abnormal results do not mean that you have cervical cancer, but that cells in your cervix could eventually become cancerous. However, finding the abnormal cells early allows for more successful treatment.
Do young women who get the HPV vaccine still need to get Pap tests?
Yes. The HPV vaccine prevents the types of HPV that cause about 9 of every 10 cervical cancers. Because the vaccine doesn't prevent all types of HPV that cause cancer, women still need to get routine Pap tests. Likewise, the vaccine doesn’t protect against types of HPV to which a person was exposed prior to vaccination.
Do people who have received the HPV vaccine still need to worry about sexually transmitted diseases?
Yes. The HPV vaccine doesn't prevent other sexually transmitted diseases such as syphilis, gonorrhea, chlamydia and herpes virus, and the HPV vaccine doesn't prevent all of the dangerous types of HPV; it prevents most of them. Vaccinated individuals should still practice safe sexual behaviors (monogamy or limiting the number of sexual partners, and condom use).
Should males get the HPV vaccine?
Yes. Males are recommended to get the HPV vaccine for two reasons:
- To protect themselves from anal and genital warts as well as cancers of the head, neck, anus, and penis.
- To reduce transmission of the virus to sexual partners.
Can the HPV vaccine treat cervical cancer?
No. Unfortunately, therapeutic trials of HPV vaccine have shown that the vaccine doesn't cause a regression in Pap smear changes that precede cervical cancer.
Relative risks and benefits
The HPV vaccine protects against certain cancers and genital warts, and it is safe. The only known side effects are mild, such as pain, redness or swelling at the injection site or low-grade fever. Therefore, the benefits of the HPV vaccine outweigh its risks.
Who
Adolescents, beginning at age 9, and teens; adults up to 45 years old who want to protect themselves
Disease risks
- Cervical cancer
- Genital warts
- Cancers of the head and neck
- Cancers of the anus and penis
- Can be fatal
Vaccine risks
- Pain, redness and tenderness at the injection site
- Low-grade fever
- Allergic reaction (1 in 1 million recipients)
References
Plotkin SA, Orenstein W, Offit PA, and Edwards KM. Human papillomavirus vaccines in Vaccines, 7th Edition. 2017, 430-455.
HPV vaccine safety concerns
HPV vaccine and autoimmune diseases
Jiang H-y, Shi, Y-d, Zhang X, et al. Human papillomavirus vaccination and the risk of autoimmune disorders: A systematic review and meta-analysis. Vaccine 2019;37:3031-3039.
Of 541 papers located, 137 were reviewed and 20 met all inclusion criteria. Five of 20 were determined to be of “low quality” based on their lack of scientific rigor. Researchers determined that the HPV vaccine did not cause increases in autoimmune disorders, including several neurological, gastrointestinal, musculoskeletal or systemic, hematological or dermatological disorders. Nor did the vaccine cause type 1 diabetes or thyroid disorders.
Bi D, Apter D, Eriksson T, Hokkanen M, Zima J, et al. Safety of the AS04-adjuvanted human papillomavirus (HPV)-16/18 vaccine in adolescents aged 12-15 years: end-of-study results from a community-randomized study up to 6.5 years. Human Vaccines and Immunotherapy 2019;12:1-12 (epub ahead of print).
In this randomized study, the authors evaluated the efficacy and safety of an adjuvanted-HPV 16/18 vaccine in more than 32,000 Finnish adolescent males and females over a 6.5-year period by comparing those who received HPV vaccine to those who received hepatitis B vaccine. The HPV vaccine adjuvant was composed of monophosphoryl-lipid A plus aluminum salts. The incidence of new-onset autoimmune diseases was similar in both vaccine groups. Similarly, those receiving HPV vaccine during pregnancy did not have an increased risk for spontaneous abortion or congenital anomalies.
Frisch M, Besson A, Clemmensen KKB, Valentiner-Branth P, Molbak K, et al. Quadrivalent human papillomavirus vaccination in boys and risk of autoimmune diseases, neurological diseases and venous thromboembolism. International Journal of Epidemiology 2018;47(2):634-641.
The authors investigated the association of quadrivalent HPV (qHPV) vaccination and the risk of 39 autoimmune diseases, 12 neurological diseases, or venous thromboembolism over a 10-year period in more than 7,000 Danish boys who received at least one dose of qHPV vaccination at the age of 10 to 17 years by comparing them to more than 560,000 boys who did not receive the vaccine. Receipt of qHPV in boys aged 10-17 years was not associated with an elevated risk of autoimmune diseases, neurological diseases, or venous thromboembolism.
Liu EY, Smith LM, Ellis A, Whitaker H, Law B, et al. Quadrivalent human papilloma virus vaccination in girls and the risk of autoimmune disorders: the Ontario Grade 8 HPV vaccine cohort study. Canadian Medical Association Journal 2018;190:E648-655.
The authors assessed the risk of autoimmune disorders following quadrivalent HPV (qHPV) vaccine among more than 290,000 eighth-grade girls eligible for Ontario’s school-based HPV vaccination program. There was no significant risk for developing an autoimmune disorder following HPV vaccination and the association was unchanged by a history of immune-mediated disorders and time since vaccination.
Grimaldi-Bensouda L, Rossignol M, Kone-Paut I, et al. Risk of autoimmune diseases and human papilloma virus (HPV) vaccines: six years of case-referent surveillance. Journal of Autoimmunity 2017; 19:84-90.
The authors found that HPV vaccine did not increase the risk of autoimmune diseases in females 11 to 25 years of age. Autoimmune diseases included central demyelination, multiple sclerosis, connective tissue disease, Guillain-Barré syndrome, type 1 diabetes, autoimmune thyroiditis, and idiopathic thrombocytopenic purpura.
Gronlund O, Herweijer E, Sundstrom K, et al. Incidence of new-onset autoimmune disease in girls and women with pre-existing autoimmune disease after quadrivalent human papillomavirus vaccination: a cohort study. Journal of Internal Medicine 2016;280:618-626.
The authors assessed whether HPV vaccination was associated with an increased incidence of new-onset autoimmune disease in more than 70,000 girls and women (10-30 years of age) with pre-existing autoimmune diseases. They found that HPV vaccination did not increase the risk of other autoimmune diseases in this patient population.
Grimaldi-Bensouda L, Guillemot D, Godeau B, et al. Autoimmune disorders and quadrivalent human papillomavirus vaccination of young female subjects. Journal of Internal Medicine 2014;275(4): 398-408.
The authors reviewed the records of female patients 14-26 years of age to determine if the HPV vaccine increased the risk of autoimmune disorders. HPV vaccine did not increase the risk of type 1 diabetes, idiopathic thrombocytopenic purpura, multiple sclerosis, Guillain-Barré syndrome, systemic lupus erythematosus (SLE), rheumatoid arthritis, juvenile arthritis, or autoimmune thyroiditis.
Arnheim-Dahlstrom L, Pasternak B, Svanstrom H, Sparen P, Hviid A. Autoimmune, neurological, and venous thromboembolic adverse events after immunisation of adolescent girls with quadrivalent human papillomavirus vaccine in Denmark and Sweden: cohort study. British Medical Journal 2013;347:f5906.
The authors assessed the risk of serious adverse events after vaccination of approximately 300,000 girls ages 10-17 years with quadrivalent HPV vaccine during a four-year period. The authors found no association between exposure to quadrivalent HPV vaccine and autoimmune, neurological or venous thromboembolic adverse events.
HPV and chronic fatigue syndrome (CFS)/systemic exertion intolerance disease (SEID)
Schurink-van’t Klooster TM, Kemmeren JM, van der Maas NAT, van de Putte EM, ter Wolbeek M, et al. No evidence found for an increased risk of long-term fatigue following human papillomavirus vaccination of adolescent girls. Vaccine 2018;36:6796-6802.
The Dutch National Institute for Public Health and the Environment investigated the relationship between HPV vaccination and chronic fatigue syndrome (CFS). Investigators compared the incidence of CFS before and after HPV vaccine administration among nearly 70,000 females during a six-year period. HPV vaccine receipt was not associated with an increased incidence of CFS. Further, the incidence of CFS did not differ before and after the introduction of HPV vaccine.
Skufca J, Ollgren J, Artama M, Ruokokoski E, Nohynek H, et al. The association of adverse events with bivalent human papillomavirus vaccination: a nationwide register-based cohort study in Finland. Vaccine 2018;36:5926-5933.
The authors evaluated the association between bivalent HPV vaccine (Cervarix®) and 65 selected autoimmune diseases and clinical syndromes during a three-year period in Finland among females ages 11-15 years. The authors reported a lower incidence of chronic recurrent pain syndrome (CRPS) and systemic exertion intolerance disease (SEID) in females who received the bivalent HPV vaccine compared with those who did not. The authors reported an increased incidence of CRPS/SEID diagnoses in the post-HPV vaccination era compared to the pre-HPV era; however, this same increased incidence was also observed in the male population who did not receive bivalent HPV vaccination.
Feiring B, Laake I, Bakken IJ, Greve-Isdahl M, Wyller VB, et al. HPV vaccination and risk of chronic fatigue syndrome/myalgic encephalomyelitis: a nationwide register-based study from Norway. Vaccine 2017;35:4203-4212.
The authors investigated the association between HPV vaccination and risk of chronic fatigue syndrome (CFS), myalgic encephalomyelitis (ME) in more than 175,000 females ages 10-17 years living in Norway during a six-year period. HPV vaccination was not associated with CFS/ME at any time following vaccination. The authors observed an increase in the incidence of CFS/ME within the Norwegian population; however, this increase was similar among girls and unvaccinated boys.
Donegan K, Beau-Lejdstrom R, King B, Seabroke S, Thomson A, et al. Bivalent human papillomavirus vaccine and the risk of fatigue syndromes in girls in the UK. Vaccine 2013;31:4961-4967.
The authors compared the incidence of fatigue syndromes in girls before and after the start of an HPV vaccination campaign that included at least 1.5 million girls receiving at least one dose. The number of spontaneous chronic fatigue reports following the use of bivalent HPV vaccine was consistent with estimated background rates. The incidence of fatigue syndromes in girls aged 12-20 years did not change after the introduction of the vaccine.
Human papillomavirus (HPV) vaccine and chronic regional pain syndromes (CRPS)
Arana JE, Harrington T, Cano M, Lewis P, Mba-Jonas A, et al. Post-licensure safety monitoring of quadrivalent human papillomavirus vaccine in the Vaccine Adverse Event Reporting System (VAERS), 2009-2015. Vaccine 2018;36:1781-1788.
The authors reviewed reports to VAERS between 2009 and 2015 in females and males aged 9-26 years who received quadrivalent HPV vaccination. More than 60 million doses of quadrivalent HPV vaccine had been distributed during this time period in the United States. The authors concluded that they did not observe any unusual or unexpected patterns of reporting of CRPS, but noted a lack of consistency in the diagnostic criteria used by healthcare providers.
Skufca J, Ollgren J, Artama M, Ruokokoski E, Nohynek H, et al. The association of adverse events with bivalent human papillomavirus vaccination: a nationwide register-based cohort study in Finland. Vaccine 2018;36:5926-5933.
The authors evaluated the association between bivalent HPV vaccine and 65 selected autoimmune diseases and clinical syndromes over a three-year period in Finland among females aged 11-15 years. The authors found no increased incidence of complex regional pain syndrome (CRPS) in those who were vaccinated with bivalent HPV vaccine versus those who did not receive the vaccine. Additionally, the authors found no increase in the incidence of CRPS in the pre- vs. post-HPV vaccine era.
Moreira Jr ED, Block SL, Ferris D, Giuliano AR, Iversen OE, et al. Safety profile of the 9-valent HPV vaccine: a combined analysis of 7 phase III clinical trials. Pediatrics 2016;138(2):e20154387.
The authors investigated the safety profile of the 9-valent human papillomavirus (9vHPV) vaccine in seven phase III studies conducted in more than 15,000 males and females aged 9 to 26 years. The authors found only two reported cases of CRPS, both of which were attributed to a previous injury.
European Medicines Agency. Pharmacovigilance Risk Assessment Committee. Assessment Report. Review under Article 20 of Regulation (EC) No 726/2004 [Internet]. Human Papillomavirus (HPV) vaccines. London: EMA;2015 Nov 11 [cited 2019 Mar 1]. Available from: https://www.ema.europa.eu/en/documents/referral/hpv-vaccines-article-20-procedure-assessment-report_en.pdf
The Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency (EMA), in response to a request from Denmark, performed an in-depth review of the safety of HPV vaccine regarding complex regional pain syndrome (CRPS) and postural orthostatic tachycardia syndrome (POTS). The PRAC concluded that the available evidence does not support that CRPS or POTS are caused by HPV vaccines.
Huygen F, Verschueren K, McCabe C, Stegmann JU, Zima J, et al. Investigating reports of complex regional pain syndrome: an analysis of HPV-16/18-adjuvanted vaccine post-licensure data. EBioMedicine 2015;2:1114-1121.
The authors investigated a potential safety signal for CRPS related to HPV-16/18-adjuvanted vaccine by reviewing six years of spontaneous reports of CRPS within GlaxoSmithKline’s central worldwide safety database in addition to a full literature review. Globally, only five cases of CRPS were confirmed by independent experts, for a reporting rate of 0.1 cases per 100,000 doses distributed. Observed CRPS incidence after HPV-16/18-adjuvanted vaccine was significantly below expected rates in the general population. No reports of CRPS were identified from clinical trials. The authors concluded there is not sufficient evidence to suggest an increased risk of developing CRPS following vaccination with HPV-16/18-adjuvanted vaccine.
HPV vaccine and postural orthostatic tachycardia syndrome (POTS)
Skufca J, Ollgren J, Artama M, Ruokokoski E, Nohynek H, et al. The association of adverse events with bivalent human papillomavirus vaccination: a nationwide register-based cohort study in Finland. Vaccine 2018;36:5926-5933.
The authors evaluated the relationship between receipt of a bivalent HPV vaccine (Cervarix®) and 65 selected autoimmune diseases during a three-year period in Finland among females ages 11-15 years. The authors found no increased incidence of POTS in those who were vaccinated compared with those who weren’t. Additionally, the authors found no increase in the incidence of POTS when comparing the pre- and post-HPV vaccine era.
Arana J, Mba-Jonas A, Jankosky C, Lewis P, Moro PL, et al. Reports of postural orthostatic tachycardia syndrome after human papillomavirus vaccination in the Vaccine Adverse Event Reporting System. J Adol Health 2017;61:577-582.
The authors reviewed postural orthostatic tachycardia syndrome (POTS) reports submitted to VAERS following HPV vaccination. Worldwide, more than 200 million doses of HPV vaccine were distributed during the nine-year period and 29 reports met POTS criteria. Within the United States, nearly 85 million HPV vaccine doses were distributed during this same time frame and 13 reports met POTS criteria, with an estimated rate of 1 POTS report for every 6.5 million HPV doses distributed. The authors found no evidence to suggest a safety problem with POTS following HPV vaccination.
European Medicines Agency. Pharmacovigilance Risk Assessment Committee. Assessment Report. Review under Article 20 of Regulation (EC) No 726/2004 [Internet]. Human Papillomavirus (HPV) vaccines. London: EMA;2015 Nov 11 [cited 2019 Mar 1].
The Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency (EMA) was charged with performing an in-depth review of the safety of HPV vaccine related to complex regional pain syndrome (CRPS) and postural orthostatic tachycardia syndrome (POTS) after Denmark had requested an investigation. The PRAC found that report of POTS cases following HPV vaccines were not greater than would have been expected in the absence of vaccination, supporting the notion that HPV vaccine does not cause POTS.
HPV vaccine and primary ovarian failure
Arana JE, Harrington T, Cano M, Lewis P, Mba-Jonas A, et al. Post-licensure safety monitoring of quadrivalent human papillomavirus vaccine in the Vaccine Adverse Event Reporting System (VAERS), 2009-2015. Vaccine 2018;36:1781-1788.
The authors evaluated reports to the Vaccine Adverse Events Reporting System (VAERS) between 2009 and 2015 in females and males aged 9-26 years who received quadrivalent HPV vaccination. More than 60 million doses of quadrivalent HPV vaccine were distributed during this time frame in the United States. Only two cases of physician-diagnosed primary ovarian insufficiency after quadrivalent HPV vaccination were reported, both in patients with a history of amenorrhea.
Naleway AL, Mittendorf KF, Irving SA, Henninger ML, Crane B, et al. Primary ovarian insufficiency and adolescent vaccination. Pediatrics 2018;142(3):e20180943.
The authors evaluated the incidence of primary ovarian insufficiency (POI) following HPV vaccination, as well as Tdap, MenACWY, and inactivated influenza vaccines, within the Kaiser Permanente Northwest database (United States) during an eight-year period. About 200,000 females were evaluated, including 60,000 who had received at least one dose of HPV vaccine. Only one confirmed case of POI was identified in a patient 23 months after her third dose of HPV vaccine. The authors found no increased risk of primary ovarian insufficiency after HPV vaccination or any other adolescent vaccination.
HPV vaccine and promiscuity
Chua GT, Ho FK, Tung KT, Wong RS, Cheong KN, et al. Sexual behaviors and intention for cervical screening among HPV-vaccinated young Chinese females. Vaccine 2019;pii: S0264-410X(19)31573-7. (epub ahead of print).
In this survey of Chinese females aged 12-27 years, receipt of at least one dose of HPV vaccine was not associated with underage sex, earlier sexual exposure, multiple sex partners or unprotected sex.
Cook EE, Venkataramani AS, Kim JJ, Tamimi RM, Holmes MD. Legislation to increase uptake of HPV vaccination and adolescent sexual behaviors. Pediatrics 2018;142(3): e20180458.
The authors compared the rates of sexual intercourse before and after the implementation of state laws regarding HPV vaccine. They found that implementation of HPV legislation was not associated with changes in adolescent sexual behaviors in the United States.
Smith LM, Kaufman JS, Strumpf EC, Lévesque LE. Effect of human papillomavirus (HPV) vaccination on clinical indicators of sexual behaviour among adolescent girls: the Ontario Grade 8 HPV Vaccine Cohort Study. CMAJ 2015;187(2):E74-E81.
The authors determined the effect of HPV vaccination on sexual behavior, including pregnancy and non-HPV-related sexually transmitted infections, in more than 260,000 adolescent girls in Ontario. They found that neither HPV vaccination nor HPV-vaccination program eligibility increased the risk of pregnancy or non-HPV-related sexually transmitted infections or both among females aged 14-17 years.
Mayhew A, Kowalczyk Mullins TL, Rosenthal SL, Zimet GD, Morrow C, et al. Risk perceptions and subsequent sexual behaviors after HPV vaccination in adolescents. Pediatrics 2014;133:404-411.
The authors determined whether sexual risk perceptions after the first HPV vaccine dose predicted subsequent sexual behaviors. Risk perceptions included perceived risk of non-HPV-related sexually transmitted infections and perceived need for safer sexual behaviors after HPV vaccination. Nearly half of all participants were sexually inexperienced; risk perceptions within this group were not associated with subsequent sexual intercourse. Among all sexually experienced participants, baseline risk perceptions were not associated with the subsequent number of sexual partners or condom use. The authors concluded that HPV vaccination does not change sexual behaviors among adolescents.
Bednarczyk RA, Davis R, Ault K, Orenstein W, Omer SB. Sexual activity-related outcomes after human papillomavirus vaccination of 11- to 12-year-olds. Pediatrics 2012;130(5):798-805.
The authors evaluated changes in the rates of sexual activity-related outcomes, including sexually transmitted infection testing or diagnosis, pregnancy testing or diagnosis, or counseling on contraceptives, in females who received HPV vaccination at the age of 11-12 years compared to similarly aged girls who did not receive the vaccine. There was no increased in the rate of sexual activity indicators in vaccinated versus unvaccinated females.
HPV vaccine and venous thromboembolism (VTE, blood clots)
Frisch M, Besson A, Clemmensen KKB, Valentiner-Branth P, Molbak K, et al. Quadrivalent human papillomavirus vaccination in boys and risk of autoimmune diseases, neurological diseases and venous thromboembolism. International Journal of Epidemiology 2018;47(2):634-641.
The authors investigated the association of quadrivalent HPV (qHPV) vaccination and the risk of 39 autoimmune diseases, 12 neurological diseases, or venous thromboembolism over a 10-year period in more than 7,000 Danish boys who received at least one dose of qHPV vaccination at the age of 10 to 17 years by comparing them to more than 560,000 boys who did not receive the vaccine. Receipt of qHPV in boys aged 10-17 years was not associated with an elevated risk of autoimmune diseases, neurological diseases, or venous thromboembolism.
Skufca J, Ollgren J, Artama M, Ruokokoski E, Nohynek H, et al. The association of adverse events with bivalent human papillomavirus vaccination: a nationwide register-based cohort study in Finland. Vaccine 2018;36:5926-5933.
The authors evaluated the association between bivalent HPV vaccine (Cervarix®) and 65 selected autoimmune diseases and clinical syndromes over a three-year period in Finland among females aged 11-15 years. The incidence of venous thromboembolism (VTE) was indistinguishable between those who received bivalent HPV and those who did not. Further, incidence of VTE in the pre- and post-bivalent HPV era was the same.
Naleway AL, Crane B, Smith N, Daley MF, Donahue J, et al. Absence of venous thromboembolism risk following quadrivalent human papillomavirus vaccination. Vaccine Safety Datalink, 2008-2011. Vaccine 2016;34:167-171.
The authors evaluated the risk of developing VTE among 9- to 26-year-old male and female subjects following quadrivalent HPV vaccine exposure. More than 1.24 million doses were administered to more than 650,000 persons during a three-year period. The authors did not find an increased risk of VTE after quadrivalent HPV vaccine receipt, and no temporal relationship was observed when different exposure periods or different age categories were analyzed. Almost all confirmed VTE cases (97 percent) had at least one known risk factor for VTE, and nearly half had three or more risk factors such as hormonal contraceptive use, obesity and hypercoagulability. The authors concluded that the risk of developing VTE among 9- to 26-year-olds was not elevated following quadrivalent HPV vaccination.
Yih Wk, Greene SK, Zichittella L, Kulldorff M, Baker MA, et al. Evaluation of the risk of venous thromboembolism after quadrivalent human papillomavirus vaccination among US females. Vaccine 2016;34:172-178.
The authors evaluated the risk of developing VTE among 9- to 26-year-old females following quadrivalent HPV vaccine. More than 1.4 million doses of vaccine were administered to more than 650,000 subjects during a seven-year period. The authors found no evidence for an increased risk of VTE, even when accounting for hormonal contraceptive use, age, VTE risk factors, and number of doses of HPV vaccines. All confirmed VTE cases had between 1 and 5 risk factors for VTE.
Scheller NM, Pasternak B, Svanstrom H, Hviid A. Quadrivalent human papillomavirus vaccine and the risk of venous thromboembolism. JAMA 2014;312(2):187-188.
The authors investigated the potential association of VTE and HPV vaccination during a seven-year period in more than 1.6 million Danish females 10 to 44 years of age, including more than 500,000 HPV vaccine recipients. No association was observed between receipt of quadrivalent HPV vaccine and VTE during the 42 days following vaccination, even when divided into shorter time periods (e.g., 1-14, 15-28, and 29-42 days) or when analyzed by age subgroup, inclusion of only anticoagulant-treated cases, inclusion of only HPV vaccine-exposed cases, or adjusting for oral contraceptive use. The authors concluded that receipt of quadrivalent HPV vaccine did not increase the risk of VTE.
Arnheim-Dahlstrom L, Pasternak B, Svanstrom H, Sparen P, Hviid A. Autoimmune, neurological, and venous thromboembolic adverse events after immunisation of adolescent girls with quadrivalent human papillomavirus vaccine in Denmark and Sweden: cohort study. BMJ 2013;347:f5906.
The authors assessed the risk of serious adverse events after vaccination of approximately 300,000 girls ages 10-17 years with quadrivalent HPV vaccine during a 4-year period. The authors found no association between exposure to quadrivalent HPV vaccine and development of VTE.
Gee J, Naleway A, Shui I, Baggs J, Yin R, et al. Monitoring the safety of quadrivalent human papillomavirus vaccine: findings from the Vaccine Safety Datalink. Vaccine 2011;29:8279-8284.
The authors investigated whether quadrivalent HPV vaccine was associated with an increased risk of 9 pre-specified adverse events, including VTE, in females 9-26 years of age over a 3-year period by comparing vaccinated females to unvaccinated historical controls. More than 600,000 doses were administered during this time and 5 subjects were found to have a confirmed diagnosis of VTE, all of whom had other risk factors such as hypercoagulable disorders, hormonal contraceptive use, smoking or obesity or both. The authors concluded that HPV vaccination did not increase the risk of VTE.
Reviewed by Paul A. Offit, MD, on August 22, 2022
