G, GJ, J Tube Complications Clinical Pathway — Inpatient
G, GJ, J Tube Complications Clinical Pathway — Inpatient
Prolapse
A prolapse of the stoma is when gastric mucosa extrudes/slips forward and is visible on the exterior portion of the skin. This generally is the result of some form of pressure (internal or external) on the stoma, such as:
- Positive pressure ventilation
- Tube sizing (layers of multiple dressings that may cause pressure on balloons, size of tube, balloon in the tract)
Patients may not be uncomfortable or in pain with a prolapse.
Differentiating Prolapse from Granulation Tissue
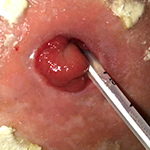
Prolapse can be difficult to identify and differentiate from hypergranulation tissue. Prolapsed gastric mucosa tends to have a beefy red color and velvety, smooth appearance. Granulation tissue tends to be pink or red in color, feels spongy or firm, and looks bumpy. If unsure about prolapse, notify the appropriate service.
Granulation Tissue

Prolapse

Prolapse
| Potential Source | Recommended Approach | Comments |
|---|---|---|
| Increased intra-abdominal pressure (e.g., positive pressure ventilation, ascites, obstruction) |
|
|
| External pressure on stoma (e.g. tube fit/sizing) |
Mild Prolapse

Severe Prolapse