What is moyamoya disease?
Moyamoya disease and moyamoya syndrome are rare but serious diseases in which the two major arteries in the front of the neck (the carotid arteries) progressively narrow. This narrowing occurs over the course of months and years, typically beginning in childhood.
The carotid arteries supply oxygen-rich blood from the heart to the brain. As they narrow, blood flow to the brain is reduced and very serious symptoms can occur, including stroke.
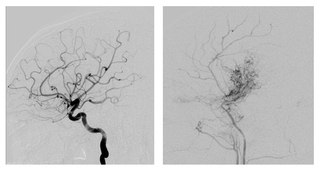
“Moyamoya” is a Japanese term (meaning “puff-puff” or “puff of smoke”) that describes how the blood vessels of a person with this condition look when evaluated with angiogram.
Causes
Moyamoya syndrome occurs in some patients who have certain chronic diseases that alter or damage blood vessels to the brain. Conditions that put children at higher risk for moyamoya syndrome include sickle cell anemia, trisomy 21 and neurofibromatosis.
Moyamoya disease refers to children who develop this blood vessel abnormality without having an underlying disease or genetic condition. In these cases, there is no known cause.
Signs and symptoms
The most common symptom that brings children to the doctor is a sudden loss of function that resembles a stroke, such as difficulty speaking or weakness of one side of the body. Learn more about the signs and symptoms of stroke in children.
Sometimes these symptoms are short-lived, resolving over a matter of hours, and no tissue damage is evident on an MRI or CT scan. Doctors call this a transient ischemic attack (TIA). Sometimes the symptoms are more long-lasting or more severe. In these cases, there may be actual tissue damage seen on a brain MRI or CT scan, which would indicate there has been a stroke and not just a TIA. When there has been a stroke, the effects are more long-lasting (days to weeks) or may even be permanent.
Treatment
At The Children’s Hospital of Philadelphia, stroke and rehabilitation specialists from the dedicated Pediatric Stroke Program work in close partnership with the pediatric neurosurgery team to provide comprehensive care for children with moyamoya disease.
Watch the video below to learn more about the treatment for moyamoya disease.
Emergency treatment for stroke in children with moyamoya disease
Immediate treatment is needed for all children with stroke no matter what the cause. The approach to treatment involves thinking of stroke and TIA as a “brain attack,” where every minute counts.
At the earliest signs or symptoms of a stroke, such as paralysis of one side of the body or loss of speaking abilities, have your child lie flat and call 911 for immediate medical care and transport to the nearest emergency room.
Immediate treatment will focus on preventing the stroke from getting worse. The EMT or emergency room team may give your child IV fluids and administer oxygen while arranging for emergency neurologic consultation and diagnostic tests such as brain MRI or CT. Our Pediatric Stroke Program has more information and resources about the initial evaluation and treatment for children with possible acute stroke.
Medical treatment for stroke in children with moyamoya disease
After the initial diagnosis and treatment of stroke or TIA, children with moyamoya disease need a variety of medical and rehabilitation therapies. These therapies are focused on preventing another stroke from occurring, and helping your child recover function. At The Children’s Hospital of Philadelphia, children who’ve experienced a stroke will be cared for by the Pediatric Stroke Program, which is designed to bring together all of the services and specialists that may be involved in your child’s stroke care.
Most children with moyamoya disease who experience a stroke will be prescribed a lifelong aspirin regimen, taken once daily to help keep the narrowed blood vessels open. Rehabilitation services such as physical therapy, occupational therapy or speech therapy are another important part of treatment for most children who have experienced a stroke.
Surgery for moyamoya disease in children
A common treatment for moyamoya disease is an indirect bypass. Two common approaches used for this type of brain surgery include pial synangiosis and encephaloduroarteriosynangiosis (EDAS). During this operation, a surgeon creates a new delivery system to bring blood to the brain.
The bone of the skull and the skin of the scalp are fed by a different set of blood vessels than the brain. In pial synangiosis, the surgeon identifies a healthy artery from this external vascular system. They then loosen a portion of an artery of the scalp, called the superficial temporal artery, and cut a circle out of the skull, with a notch on either side (see image below on the left).
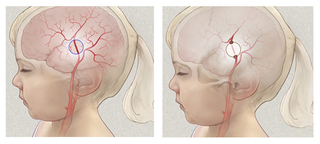
Next, the surgeon places the loose section of the artery directly onto the brain, and replaces the notched portion of skull. The notches allow the artery to go through the skull, from scalp to brain, on either side (see image above on the right.
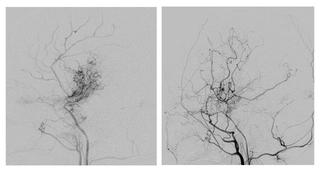
Because the brain is hungry for oxygen, the portion of the superficial temporal artery that is on the brain will sprout many branches. Think of a seedling in the ground, sprouting more and more roots. This creates an alternate system for blood delivery to the brain.
It takes months for the new vessels to form. The neurosurgeon will assess the result of the surgery through an angiogram around 12 months after surgery.
Follow-up care
Children with moyamoya disease or moyamoya syndrome will receive coordinated follow-up care from the Pediatric Stroke Program team and the neurosurgery team. Your child’s follow-up care will be tailored to her individual needs and those of your family.
After hospitalization and surgery, most children will return for an initial follow-up visit within several weeks after discharge to monitor their recovery. Provided your child is medically stable and able to tolerate these activities, rehabilitation therapy may begin during your child’s hospital stay and continue after discharge.
If your child has indirect bypass surgery, she will return to her neurosurgeon approximately one year after surgery for an angiogram.
Your child will also return for periodic follow-up appointments with the Stroke Program team. At each clinic visit, your child will be seen by the stroke neurologist, nurse, social worker, education specialist and neuropsychologist. If needed, she may also be seen by one or more of the Stroke Program’s rehabilitation therapists (PT, OT, speech therapy) to provide expert recommendations on her therapy program.
The schedule of visits spreads out to once or twice per year, depending on your child’s recovery and health needs, and continues throughout her childhood years to assure maximal recovery and developmental potential can be reached.
A child’s stroke affects everyone in the family, and our team is here to support you as you adapt to your child’s medical condition and treatment program. The Pediatric Stroke Program provides education and support for families of children with stroke and encourages active involvement of the family in all phases of care, including advocating for their child’s needs in the community setting.
Members of the Stroke team will continue to assist you and your child in the recovery process and help your child to return to a more normal lifestyle as soon as possible. We can help with adjustments to your home regimen and physical and recreation activities. If your child is school age, we will also work with your child’s school to recommend any changes needed to your child’s curriculum and school day.
Outlook
The majority of children receiving the combination of medical and surgical therapy for moyamoya disease have a good outcome, with a low risk of recurrent stroke. Restoring blood flow to the brain is an important step in maximizing their recovery of function. Surgery can be very effective in delivering blood to the brain and improving function.
This improved function will allow your child to get the most out of rehabilitation services and educational support upon return to school. Your child’s care and rehabilitation takes teamwork and dedication from healthcare providers and parents alike. CHOP’s Pediatric Stroke Program provides education and support for families of children with strokes and encourages active involvement of the family in all phases of care.
Resources to help
Moyamoya Disease Resources
Pediatric Stroke Program Resources
We have created resources to help you find answers to your questions and feel confident with the care you are providing your child.
Reviewed by Phillip B. Storm, MD
