Conducting a Productive Video Visit
Telemedicine is booming. As we “stay at home” to slow the spread of the new coronavirus disease (COVID-19) we can still care for our patients. Providers can employ telemedicine in appropriate situations to connect with patients using a secure video connection.
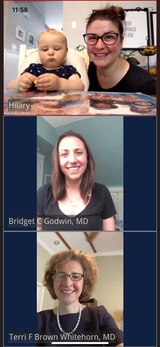
At Children's Hospital of Philadelphia (CHOP), since the start of COVID-19 restrictions, approximately half of our outpatient visits have been converted to video visits. If you are considering using telemedicine or have already jumped in, the following tips from CHOP providers could be helpful to make the experience the most productive it can be. “We are all learning how to we can best utilize telehealth for our visits,” says Paul Ufberg, DO, MBA, an attending physician in the Division of Gastroenterology, Hepatology and Nutrition. Patients, parents and providers are all in this together.
Preparation
- Set the stage for your visits. Treat the telehealth visit the same as you would an office visit. Organize an “exam room” space that is appropriate for you to talk to patients in a professional setting. Make sure that anything your patient can see is appropriate. “I moved my wedding pictures and hung my diplomas in the background,” notes Ufberg.
- Prep chart the day before. Terri F. Brown-Whitehorn, MD, an attending physician with the Division of Allergy and Immunology, considers this one of the most important steps. “That way I know what has happened since last seen,” she explains. It’s one less thing to think about when you’re about to sign on to the visit. “When I enter a visit, part of my note is completed.”
- Reboot your mobile device every few days. Doing a hard shut down and power back up will help clear out open apps that might be causing your device to lag.
- Update your video app. Make sure your Epic Haiku or Canto apps are updated. If you are using other apps to do video visits, make sure you have the latest version of those apps installed.
- Consider expanding the length of a visit. “Instead of seeing patients every 30 minutes, I see them every 45 minutes on average,” says Brown-Whitehorn. “This has been helpful in the event that there is something unexpected that has happened or if I or the parents have issues connecting.”
- Encourage and reassure hesitant families. When applicable, video visits can be as productive as office visits, but some families might be hesitant. Encourage families to give it a try. Ask them if they have concerns that you can address (like assuring them that the visits are not being recorded, etc.). In certain situations — for example, children with chronic medical issues or transportation issues (those requiring equipment) — a video visit is actually much easier and safer.
Conducting the visit
- Address that elephant in the room immediately. Explain to the patient that this will be different than other visits, and that we are ready for that. Acknowledge the limitations — “I can’t feel your belly, but maybe your parent can” and “It’s hard to see what you are describing” and “Perhaps we need to be in the same room to evaluate that better” are all reasonable things to say. Asking a parent to point out any concerns they have is also helpful.
- Be prepared for glitches. If you’re having trouble seeing something that the patient is trying to show you, it’s fine to ask for better lighting or a different view. Remember that parents or patients probably have a flashlight on their phone. Difficulties with the connection might occur, but if you are open and honest with the family about this being new, we've found many to be understanding. If a connection problem arises, be prepared to call the family.
- Make eye contact. A video visit may feel awkward at first, but it’s important to be as “present” as possible. Make sure your camera is at eye level to enhance eye contact, which is key to communication.
- Explain what you’re doing. For example, let the patient know that when you look away from the screen that you are writing notes on another computer or screen.
- Wrap up the visit. Donna Stephenson, MD, an attending physician and Medical Director of Operations and Outreach for the Division of Neurology, suggests a structure for ending each visit. “Outline your impression and plan, and make sure the family understands and is in agreement,” she says. “Create and make available an after-visit summary with detailed written instructions. Ask for feedback, and end with a smile!”
Overall considerations
- Build up slowly. For the first few days or weeks, see what works and what does not. Then add more as your comfort level grows.
- A video visit can be a preliminary step. One of Brown-Whitehorn’s patients thought that testing was needed to figure out a plan for a certain condition. “At times, this is the case, and we could hold off on visit,” she explains. “However, we do not need to do testing to come up with a plan to help child in the short term. We can listen to the patient’s story and see if testing is even warranted. Also, if I know the story already, it may make actual visits in person a bit more efficient.” But there’s a caveat: If the thought of two copays is an issue, then waiting for an in-person visit may make more financial sense for that family.
- Reconsider your work hours. Can your schedule accommodate more patients or different hours? “I used to drive 30 to 45 minutes to work every day, but I do not have to now,” says Ufberg. He now uses that former commute time to see another 1-2 patients, have a meeting — or just walk the dog. Make adjustments that work for you.