
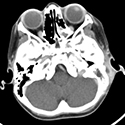
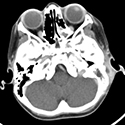
A 4-year-old otherwise healthy girl presented to the ED after 10 days of left ear pain, daily high-grade fevers, and muscle aches. She was seen by her pediatrician 8 days earlier and diagnosed with a viral upper respiratory infection. One day before presentation, her ear started protruding, and she developed swelling and redness behind the ear. On ED evaluation, she was found to have left ear proptosis and postauricular edema, erythema, and tenderness. CT temporal bone scan (see Figure 1) showed evidence of coalescent left mastoiditis (1A) with postauricular subperiosteal abscess (SPA) and thickened dura over the sigmoid sinus (1B).
She was started on broad-spectrum IV antibiotics and taken to the OR the following day for incision and drainage of SPA, simple mastoidectomy, and bilateral myringotomy and tube placement.
In the OR, she was found to have purulent fluid in the subperiosteal layer, and focal erosion of the mastoid cortical bone and sigmoid plate.
Infectious Diseases recommended 3 weeks of cephalexin for penicillin-resistant Staphylococcus. She was discharged on hospital day 5, and on follow-up her mastoiditis had completely resolved with normal hearing on audiogram.
Acute mastoiditis (AM) is the most common complication of acute otitis media (AOM) and is often seen by my co-fellows and me, especially during the winter months. It can present in up to 0.4% of AOM cases, mainly in the pediatric population. Extracranially, AM may be complicated by SPA, facial nerve palsy, labyrinthitis, or internal jugular vein thrombosis. Prompt diagnosis and treatment is important, as AM can progress intracranially leading to sigmoid sinus thrombosis, meningitis, encephalitis, or intracranial abscess. Notably, AM must be distinguished from “otomastoiditis,” which is a catch-all term often used by radiologists to describe any acute or chronic otitis causing opacification of the mastoid air cells on imaging. By contrast, AM represents an acute, severe complication of AOM causing bony destruction and coalescence of the mastoid air cells.
The diagnosis of AM is made clinically, with signs and symptoms of recent AOM, protrusion of the pinna, and postauricular tenderness, edema, and/or erythema. If there is concern for complicated AM, CT and/or MR imaging is essential in defining disease extent. Treatment varies according to disease severity, and includes IV antibiotics, myringotomy +/- tympanostomy tube placement, SPA drainage, and/or simple mastoidectomy. Surgical intervention is typically reserved for cases of complicated AM or lack of improvement on antibiotics alone. With early initiation of antibiotic therapy, AM can resolve without the development of severe complications.
Reference and selected reading
Anne S et al. Medical versus surgical treatment of pediatric acute mastoiditis: a systematic review. Laryngoscope. 2019;129(3):754-760.
Rosenfeld RM, Tunkel DE, Schwartz SR, et al. Clinical practice guideline: tympanostomy tubes in children (update), Otolaryngol Head Neck Surg. 2022;166(1_suppl):S1-S55.
Allan S. Lieberthal A, Carroll A, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013:131(3):e964–e999.

A 4-year-old otherwise healthy girl presented to the ED after 10 days of left ear pain, daily high-grade fevers, and muscle aches. She was seen by her pediatrician 8 days earlier and diagnosed with a viral upper respiratory infection. One day before presentation, her ear started protruding, and she developed swelling and redness behind the ear. On ED evaluation, she was found to have left ear proptosis and postauricular edema, erythema, and tenderness. CT temporal bone scan (see Figure 1) showed evidence of coalescent left mastoiditis (1A) with postauricular subperiosteal abscess (SPA) and thickened dura over the sigmoid sinus (1B).
She was started on broad-spectrum IV antibiotics and taken to the OR the following day for incision and drainage of SPA, simple mastoidectomy, and bilateral myringotomy and tube placement.
In the OR, she was found to have purulent fluid in the subperiosteal layer, and focal erosion of the mastoid cortical bone and sigmoid plate.
Infectious Diseases recommended 3 weeks of cephalexin for penicillin-resistant Staphylococcus. She was discharged on hospital day 5, and on follow-up her mastoiditis had completely resolved with normal hearing on audiogram.
Acute mastoiditis (AM) is the most common complication of acute otitis media (AOM) and is often seen by my co-fellows and me, especially during the winter months. It can present in up to 0.4% of AOM cases, mainly in the pediatric population. Extracranially, AM may be complicated by SPA, facial nerve palsy, labyrinthitis, or internal jugular vein thrombosis. Prompt diagnosis and treatment is important, as AM can progress intracranially leading to sigmoid sinus thrombosis, meningitis, encephalitis, or intracranial abscess. Notably, AM must be distinguished from “otomastoiditis,” which is a catch-all term often used by radiologists to describe any acute or chronic otitis causing opacification of the mastoid air cells on imaging. By contrast, AM represents an acute, severe complication of AOM causing bony destruction and coalescence of the mastoid air cells.
The diagnosis of AM is made clinically, with signs and symptoms of recent AOM, protrusion of the pinna, and postauricular tenderness, edema, and/or erythema. If there is concern for complicated AM, CT and/or MR imaging is essential in defining disease extent. Treatment varies according to disease severity, and includes IV antibiotics, myringotomy +/- tympanostomy tube placement, SPA drainage, and/or simple mastoidectomy. Surgical intervention is typically reserved for cases of complicated AM or lack of improvement on antibiotics alone. With early initiation of antibiotic therapy, AM can resolve without the development of severe complications.
Reference and selected reading
Anne S et al. Medical versus surgical treatment of pediatric acute mastoiditis: a systematic review. Laryngoscope. 2019;129(3):754-760.
Rosenfeld RM, Tunkel DE, Schwartz SR, et al. Clinical practice guideline: tympanostomy tubes in children (update), Otolaryngol Head Neck Surg. 2022;166(1_suppl):S1-S55.
Allan S. Lieberthal A, Carroll A, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013:131(3):e964–e999.