Eva Catenaccio, MD
Case: A 6-month-old previously healthy girl presents with 4 days of abnormal movements. Initially her mother noticed isolated episodes of the patient opening her eyes very wide. These progressed into episodes where she would suddenly lift her arms above her head and cry out. The movements have increased in frequency and started to occur in clusters over the past 2 days. She has otherwise been breastfeeding and acting normally. She was born full term after a healthy pregnancy. She has met her developmental milestones on time. Her physical exam is notable for several hypomelanotic macules, but is otherwise normal.
Discussion: Diagnoses to consider in this case of a 6-month-old with stereotyped episodes of eye widening and sudden arm elevation include seizures and benign neonatal movements, such as shuddering spells or stereotypies. In a child under 2 years of age, these events are particularly concerning for infantile spasms, a type of seizure that typically manifest as brief episodes of truncal flexion with arm extension and elevation occurring in clusters often around sleep/wake transitions. Children often cry with the spasms. Infantile spasms can be associated with developmental regression and a specific pattern of brain activity called hypsarrhythmia. This combination is referred to as infantile spasms syndrome (previously West syndrome), an epileptic encephalopathy characterized by both seizures and cognitive and developmental impairments.
Key to diagnosis: hypomelanotic macules
The exam in children with infantile spasms is often normal. However, this patient had hypomelanotic macules on exam, which is suggestive of an underlying diagnosis of tuberous sclerosis complex (TSC). TSC is a neurocutaneous disorder caused by a pathogenic variant in either the TSC1
or TSC2
genes. These genes encode hamartin and tuberin, proteins involved in a regulation of cell growth.
Children with TSC can have abnormal growths in multiple tissues, including the brain, where they are called cortical tubers. Infantile spasms occur in up to two-thirds of children with TSC, and up to a quarter of patients with infantile spasms are found to have TSC. Other etiologies of infantile spasms syndrome include: cerebral malformations, brain injuries (infection, stroke, hypoxic ischemic encephalopathy, traumatic brain injury), inherited metabolic conditions, and other genetic conditions. If left untreated the spasms and hypsarrhythmia do eventually resolve by 3 to 5 years of age, but these children develop multiple other seizure types and intellectual disability.
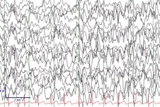
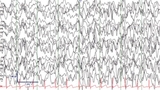
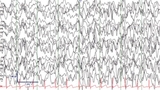
Though rare, infantile spasms are important to recognize and treat early to try to prevent developmental consequences and reduce risk of future epilepsy. Spasms can be subtle and easily confused for normal infant movements. Thus, a child with events concerning for infantile spasms warrants a rapid evaluation with electroencephalography (EEG) to capture events of concern and evaluate for hypsarrhythmia. See Figure 1.
Additional confirmation tests
If the diagnosis is not clear on the initial EEG, repeat or prolonged monitoring may show hypsarrhythmia. Once the diagnosis is confirmed on EEG, additional testing to determine the etiology of the infantile spasms typically includes magnetic resonance imaging (MRI) followed by genetic and metabolic testing if no etiology is identified. With the widespread use of MRI and genetic/metabolic testing, an etiology is identified in most cases; these are termed symptomatic infantile spasms.
In this case, detection of cortical tubers supported a TSC diagnosis, which was confirmed with genetic testing. Effective treatment of infantile spasms within the first few weeks of symptom onset is associated with an improved prognosis, particularly in cases where there is no identified underlying cause (cryptogenic). For symptomatic cases, the underlying etiology is often the most important driver of the child’s ultimate outcome in terms of development and epilepsy.
Treatment
The first-line treatment for infantile spasms is hormonal therapy, which can be administered either as injections of adrenocorticotropic hormone (ACTH) or oral corticosteroids. Major side effects include hypertension, irritability, gastrointestinal bleeding, increased appetite, increased susceptibility to infection, and hypothalamus-pituitary axis suppression.
Vigabatrin, an antiseizure medication, is typically considered the second- line agent except in patients with TSC for whom it is the first-line treatment. Vigabatrin is a GABA-transaminase inhibitor and leads to increased GABA, an inhibitory neurotransmitter, in the central nervous system. Major side effects include sedation, retinal toxicity leading to peripheral vision loss, and white matter changes of unclear significance.
In this child with suspected TSC, combination therapy with oral prednisolone and vigabatrin was initiated as soon as the diagnosis of infantile spasms was confirmed on EEG. However, after the MRI confirmed the suspected diagnosis of TSC, corticosteroid therapy was discontinued. The clinical spasms resolved within 24 hours of initiation of treatment and the follow-up EEG after 2 weeks of treatment showed resolution of the hypsarrhythmia, though with ongoing epileptiform abnormalities. Despite resolution of the infantile spasms, this child eventually went on to develop focal onset seizures, which is common in children with TSC.
Featured in this article
Specialties & Programs
Eva Catenaccio, MD
Case: A 6-month-old previously healthy girl presents with 4 days of abnormal movements. Initially her mother noticed isolated episodes of the patient opening her eyes very wide. These progressed into episodes where she would suddenly lift her arms above her head and cry out. The movements have increased in frequency and started to occur in clusters over the past 2 days. She has otherwise been breastfeeding and acting normally. She was born full term after a healthy pregnancy. She has met her developmental milestones on time. Her physical exam is notable for several hypomelanotic macules, but is otherwise normal.
Discussion: Diagnoses to consider in this case of a 6-month-old with stereotyped episodes of eye widening and sudden arm elevation include seizures and benign neonatal movements, such as shuddering spells or stereotypies. In a child under 2 years of age, these events are particularly concerning for infantile spasms, a type of seizure that typically manifest as brief episodes of truncal flexion with arm extension and elevation occurring in clusters often around sleep/wake transitions. Children often cry with the spasms. Infantile spasms can be associated with developmental regression and a specific pattern of brain activity called hypsarrhythmia. This combination is referred to as infantile spasms syndrome (previously West syndrome), an epileptic encephalopathy characterized by both seizures and cognitive and developmental impairments.
Key to diagnosis: hypomelanotic macules
The exam in children with infantile spasms is often normal. However, this patient had hypomelanotic macules on exam, which is suggestive of an underlying diagnosis of tuberous sclerosis complex (TSC). TSC is a neurocutaneous disorder caused by a pathogenic variant in either the TSC1
or TSC2
genes. These genes encode hamartin and tuberin, proteins involved in a regulation of cell growth.
Children with TSC can have abnormal growths in multiple tissues, including the brain, where they are called cortical tubers. Infantile spasms occur in up to two-thirds of children with TSC, and up to a quarter of patients with infantile spasms are found to have TSC. Other etiologies of infantile spasms syndrome include: cerebral malformations, brain injuries (infection, stroke, hypoxic ischemic encephalopathy, traumatic brain injury), inherited metabolic conditions, and other genetic conditions. If left untreated the spasms and hypsarrhythmia do eventually resolve by 3 to 5 years of age, but these children develop multiple other seizure types and intellectual disability.
Though rare, infantile spasms are important to recognize and treat early to try to prevent developmental consequences and reduce risk of future epilepsy. Spasms can be subtle and easily confused for normal infant movements. Thus, a child with events concerning for infantile spasms warrants a rapid evaluation with electroencephalography (EEG) to capture events of concern and evaluate for hypsarrhythmia. See Figure 1.
Additional confirmation tests
If the diagnosis is not clear on the initial EEG, repeat or prolonged monitoring may show hypsarrhythmia. Once the diagnosis is confirmed on EEG, additional testing to determine the etiology of the infantile spasms typically includes magnetic resonance imaging (MRI) followed by genetic and metabolic testing if no etiology is identified. With the widespread use of MRI and genetic/metabolic testing, an etiology is identified in most cases; these are termed symptomatic infantile spasms.
In this case, detection of cortical tubers supported a TSC diagnosis, which was confirmed with genetic testing. Effective treatment of infantile spasms within the first few weeks of symptom onset is associated with an improved prognosis, particularly in cases where there is no identified underlying cause (cryptogenic). For symptomatic cases, the underlying etiology is often the most important driver of the child’s ultimate outcome in terms of development and epilepsy.
Treatment
The first-line treatment for infantile spasms is hormonal therapy, which can be administered either as injections of adrenocorticotropic hormone (ACTH) or oral corticosteroids. Major side effects include hypertension, irritability, gastrointestinal bleeding, increased appetite, increased susceptibility to infection, and hypothalamus-pituitary axis suppression.
Vigabatrin, an antiseizure medication, is typically considered the second- line agent except in patients with TSC for whom it is the first-line treatment. Vigabatrin is a GABA-transaminase inhibitor and leads to increased GABA, an inhibitory neurotransmitter, in the central nervous system. Major side effects include sedation, retinal toxicity leading to peripheral vision loss, and white matter changes of unclear significance.
In this child with suspected TSC, combination therapy with oral prednisolone and vigabatrin was initiated as soon as the diagnosis of infantile spasms was confirmed on EEG. However, after the MRI confirmed the suspected diagnosis of TSC, corticosteroid therapy was discontinued. The clinical spasms resolved within 24 hours of initiation of treatment and the follow-up EEG after 2 weeks of treatment showed resolution of the hypsarrhythmia, though with ongoing epileptiform abnormalities. Despite resolution of the infantile spasms, this child eventually went on to develop focal onset seizures, which is common in children with TSC.
Contact us
Division of Neurology