A healthy 11-year-old girl was referred to the neuro-ophthalmology service for abnormal optic nerves. She had recently been complaining of difficulty seeing the board at school and was seen by a local ophthalmologist who noted optic nerve head elevation. She did not complain of headache, transient visual obscurations, pulsatile tinnitus or vision loss. Her weight and BMI were in the 50th percentile for age and she denied recent weight gain or use of any medications.
A full neuro-ophthalmologic exam was done and revealed normal visual acuity, color vision and visual fields full to confrontation. Her pupils were symmetric without evidence of a relative afferent defect. Anterior segment exam was normal and the dilated fundus exam demonstrated elevated nerves bilaterally. The optic nerve margins were blurred (Image 2) without vessel obscuration, hemorrhage, Paton’s lines and nerve fiber layer infarcts (cotton wool spots).
- What is the presumed diagnosis?
- What is the management plan?
Answers
The examination is significant for optic nerve head elevation. The two most common etiologies on the differential diagnosis include papilledema and pseudopapilledema secondary to drusen. In our patient, the lack of vessel obscuration, symptoms and other risk factors for elevated intracranial pressure (ICP) favors a diagnosis of optic nerve head drusen. Drusen are small, round, often calcified hyaline bodies located in the optic nerve head tissue. Typically asymptomatic, they can cause visual field defects on formal testing.
Evaluating a patient for optic nerve head elevation should always include a thorough history to identify symptoms of elevated ICP such as headache that is frequently worse in the morning or while lying flat, transient visual obscurations, and pulsatile tinnitus. Risk factors for elevated intracranial pressure include obesity, medications such as chronic steroids, minocycline, vitamin A or Accutane, and exposure to certain infections such as Lyme disease. Beyond the comprehensive examination, additional diagnostic studies should include B-scan ultrasound and visual field testing.
B-scan ultrasound is an easy, noninvasive assessment that can be performed in virtually all ages. As it did in our patient (Image 1), it will highlight calcification within drusen. If B-scan ultrasound does not identify drusen as the cause for the optic nerve head elevation, true papilledema may be more likely and require urgent neuro-imaging. If the patient is symptomatic (e.g., headache, pulsatile tinnitus), and the B-scan identifies drusen, neuro-imaging may still be indicated as both papilledema and drusen can coexist. Additional ophthalmic testing may be beneficial, including fundus photography and optical coherence tomography to monitor the retinal nerve fiber layer thickness.
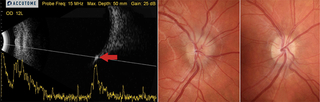
Image 1 (left): Longitudinal B-scan of the patient’s right eye demonstrates optic nerve head elevation and a hyper-reflective lesion, which persists at low gain, consistent with drusen (red arrow).
Image 2 (center): Corresponding fundus photograph of the patient’s elevated optic nerve with blurred margins.
Image 3 (right): A representative normal optic nerve photograph.
Featured in this article
Specialties & Programs
A healthy 11-year-old girl was referred to the neuro-ophthalmology service for abnormal optic nerves. She had recently been complaining of difficulty seeing the board at school and was seen by a local ophthalmologist who noted optic nerve head elevation. She did not complain of headache, transient visual obscurations, pulsatile tinnitus or vision loss. Her weight and BMI were in the 50th percentile for age and she denied recent weight gain or use of any medications.
A full neuro-ophthalmologic exam was done and revealed normal visual acuity, color vision and visual fields full to confrontation. Her pupils were symmetric without evidence of a relative afferent defect. Anterior segment exam was normal and the dilated fundus exam demonstrated elevated nerves bilaterally. The optic nerve margins were blurred (Image 2) without vessel obscuration, hemorrhage, Paton’s lines and nerve fiber layer infarcts (cotton wool spots).
- What is the presumed diagnosis?
- What is the management plan?
Answers
The examination is significant for optic nerve head elevation. The two most common etiologies on the differential diagnosis include papilledema and pseudopapilledema secondary to drusen. In our patient, the lack of vessel obscuration, symptoms and other risk factors for elevated intracranial pressure (ICP) favors a diagnosis of optic nerve head drusen. Drusen are small, round, often calcified hyaline bodies located in the optic nerve head tissue. Typically asymptomatic, they can cause visual field defects on formal testing.
Evaluating a patient for optic nerve head elevation should always include a thorough history to identify symptoms of elevated ICP such as headache that is frequently worse in the morning or while lying flat, transient visual obscurations, and pulsatile tinnitus. Risk factors for elevated intracranial pressure include obesity, medications such as chronic steroids, minocycline, vitamin A or Accutane, and exposure to certain infections such as Lyme disease. Beyond the comprehensive examination, additional diagnostic studies should include B-scan ultrasound and visual field testing.
B-scan ultrasound is an easy, noninvasive assessment that can be performed in virtually all ages. As it did in our patient (Image 1), it will highlight calcification within drusen. If B-scan ultrasound does not identify drusen as the cause for the optic nerve head elevation, true papilledema may be more likely and require urgent neuro-imaging. If the patient is symptomatic (e.g., headache, pulsatile tinnitus), and the B-scan identifies drusen, neuro-imaging may still be indicated as both papilledema and drusen can coexist. Additional ophthalmic testing may be beneficial, including fundus photography and optical coherence tomography to monitor the retinal nerve fiber layer thickness.
Image 1 (left): Longitudinal B-scan of the patient’s right eye demonstrates optic nerve head elevation and a hyper-reflective lesion, which persists at low gain, consistent with drusen (red arrow).
Image 2 (center): Corresponding fundus photograph of the patient’s elevated optic nerve with blurred margins.
Image 3 (right): A representative normal optic nerve photograph.
Contact us
Division of Ophthalmology