In our busy CHOP Ophthalmology practice, we see many aphakic (an eye without the natural crystalline lens) children. Most were infants born with congenital or infantile cataracts who had their cloudy lens removed to clear the visual axis in the first few months of life. Unlike older children and adults, these babies did not have an intraocular lens placed in the eye. This is standard practice because infant eyes in which an intraocular lens is placed have a significantly higher rate of complications and need for further surgery, and they have not been shown to have improved visual outcomes.
The natural lens of the eye provides significant power to put the eye in focus, much like the lens of a camera. If removed and not replaced with an intraocular lens, the young child requires powerful aphakic glasses or contact lenses to put the eye in focus. These glasses and contacts can be cumbersome for some children, and families often elect to have intraocular lenses placed in the eye when the child is older, allowing the eye to be in focus without the thick glasses or contacts.
Typically, during the original cataract surgery, a peripheral ring of the lens capsule is left in the eye for this purpose. This ring allows good structural support to secure an intraocular lens when one needs to be placed.
However, a small subgroup of aphakic children are missing this support providing ring and its accompanying cables (zonules) that hold it all in place. These are children who either suffered a severe eye trauma that damaged the lens and zonules or those whose lens became dislocated due to an underlying condition.
This is most often seen in Marfan syndrome, a disease where a mutation in the FBN1 gene causes a defect in the creation of the protein fibrillin-1. The reduction in fibrillin-1 causes a decrease in the production of microfibrils, critical elastic connective tissues used throughout the body. As a result, the zonules of the eye stretch or break, and the lens in these patients will dislocate out of the visual axis, causing significant visual impairment (see Figure 5).
Whether it is trauma or a dislocated lens, these children undergo surgery where the entirety of the lens and its supporting zonules are removed, leaving the eye with inadequate support for the traditional methods of placing an intraocular lens.
Historically, when an intraocular lens placement was necessary or desired in these cases, it could be sewn to the sclera or iris. But this is a complex procedure, with the potential for a variety of difficult complications, including suture breakage years later, which allows the plastic lens to fall back into the eye.
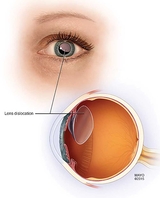
In 1978, Jan Worst, MD, of the Netherlands developed an iris claw lens that evolved over decades to the Artisan Lens produced by Ophtec. The Artisan Lens is placed on the anterior surface of the iris, and iris tissue is clipped through small claws at each end of the lens (see Figures 6 and 7). It is a relatively simple procedure compared to the suture secured intraocular lenses, and ideal for patients without adequate support for the traditional methods of securing an intraocular lens. By being secured to the iris, the lens is centered over the pupil and focuses the eye.
Although used extensively in other countries, the Artisan Lens is not approved by the Food and Drug Administration (FDA) for use in the United States. To gain access to this revolutionary lens, CHOP joined 15 other sites in a North American IRB-approved trial for implantation of this lens. The trial is evaluating North American outcomes following implantation of the Artisan Lens in pediatric patients and hopefully will lead to FDA approval for its use.
To date, the lens has been well tolerated and long lasting, with excellent visual outcomes.
The CHOP principal investigator for this study, William Anninger, MD, is actively enrolling patients for the trial.
References and suggested readings
Plager DA, Lynn MJ, Buckley EG, et al. Complications in the first 5 years following cataract surgery in infants with and without intraocular lens implantation in the Infant Aphakia Treatment Study. Am J Ophthalmol. 2014 Nov;158(5):892-898.
Buckley EG, Paediatric sutured intraocular lenses: trouble waiting to happen. Am J Ophthalmol. 2009;147:3-4.
The Artisan Aphakia Intraocular Lens in the Paediatric Eye. Sminia, ML. 2012. University of Amsterdam Digital Academic Repository website. https://pure.uva.nl/ws/files/1610830/103070_07.pdf. (Accessed December 2, 2019.)
Featured in this article
Specialties & Programs
In our busy CHOP Ophthalmology practice, we see many aphakic (an eye without the natural crystalline lens) children. Most were infants born with congenital or infantile cataracts who had their cloudy lens removed to clear the visual axis in the first few months of life. Unlike older children and adults, these babies did not have an intraocular lens placed in the eye. This is standard practice because infant eyes in which an intraocular lens is placed have a significantly higher rate of complications and need for further surgery, and they have not been shown to have improved visual outcomes.
The natural lens of the eye provides significant power to put the eye in focus, much like the lens of a camera. If removed and not replaced with an intraocular lens, the young child requires powerful aphakic glasses or contact lenses to put the eye in focus. These glasses and contacts can be cumbersome for some children, and families often elect to have intraocular lenses placed in the eye when the child is older, allowing the eye to be in focus without the thick glasses or contacts.
Typically, during the original cataract surgery, a peripheral ring of the lens capsule is left in the eye for this purpose. This ring allows good structural support to secure an intraocular lens when one needs to be placed.
However, a small subgroup of aphakic children are missing this support providing ring and its accompanying cables (zonules) that hold it all in place. These are children who either suffered a severe eye trauma that damaged the lens and zonules or those whose lens became dislocated due to an underlying condition.
This is most often seen in Marfan syndrome, a disease where a mutation in the FBN1 gene causes a defect in the creation of the protein fibrillin-1. The reduction in fibrillin-1 causes a decrease in the production of microfibrils, critical elastic connective tissues used throughout the body. As a result, the zonules of the eye stretch or break, and the lens in these patients will dislocate out of the visual axis, causing significant visual impairment (see Figure 5).
Whether it is trauma or a dislocated lens, these children undergo surgery where the entirety of the lens and its supporting zonules are removed, leaving the eye with inadequate support for the traditional methods of placing an intraocular lens.
Historically, when an intraocular lens placement was necessary or desired in these cases, it could be sewn to the sclera or iris. But this is a complex procedure, with the potential for a variety of difficult complications, including suture breakage years later, which allows the plastic lens to fall back into the eye.
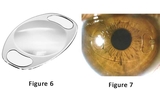
In 1978, Jan Worst, MD, of the Netherlands developed an iris claw lens that evolved over decades to the Artisan Lens produced by Ophtec. The Artisan Lens is placed on the anterior surface of the iris, and iris tissue is clipped through small claws at each end of the lens (see Figures 6 and 7). It is a relatively simple procedure compared to the suture secured intraocular lenses, and ideal for patients without adequate support for the traditional methods of securing an intraocular lens. By being secured to the iris, the lens is centered over the pupil and focuses the eye.
Although used extensively in other countries, the Artisan Lens is not approved by the Food and Drug Administration (FDA) for use in the United States. To gain access to this revolutionary lens, CHOP joined 15 other sites in a North American IRB-approved trial for implantation of this lens. The trial is evaluating North American outcomes following implantation of the Artisan Lens in pediatric patients and hopefully will lead to FDA approval for its use.
To date, the lens has been well tolerated and long lasting, with excellent visual outcomes.
The CHOP principal investigator for this study, William Anninger, MD, is actively enrolling patients for the trial.
References and suggested readings
Plager DA, Lynn MJ, Buckley EG, et al. Complications in the first 5 years following cataract surgery in infants with and without intraocular lens implantation in the Infant Aphakia Treatment Study. Am J Ophthalmol. 2014 Nov;158(5):892-898.
Buckley EG, Paediatric sutured intraocular lenses: trouble waiting to happen. Am J Ophthalmol. 2009;147:3-4.
The Artisan Aphakia Intraocular Lens in the Paediatric Eye. Sminia, ML. 2012. University of Amsterdam Digital Academic Repository website. https://pure.uva.nl/ws/files/1610830/103070_07.pdf. (Accessed December 2, 2019.)
Contact us
Division of Ophthalmology