Nasolacrimal duct obstruction (NLDO) is common in the pediatric population. Lacrimal sac massages and/or antibiotic ointment are typically recommended for children under the age of 1. Dacryocystorhinostomy (DCR) is generally recommended for treatment of congenital NLDO when a prior probing with stent placement has failed, or in the setting of dacryocystitis (an infection of the lacrimal sac).
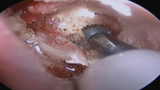
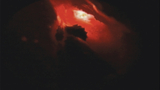
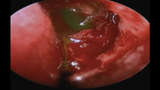
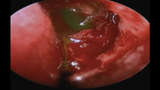
The surgical technique for DCR traditionally required a skin incision over the lacrimal sac. However, the newer technique does not and, as shown in the photos to the right, involves the use of an endoscopic camera to visualize the intranasal space. A light pipe is used to cannulate the proximal tear system and lacrimal sac via the upper or lower punctum, and this transilluminates through the nasal mucosa. With the help of direct endoscopic visualization in the nose, the area of the lacrimal sac fossa is identified as it illuminates (Image 1). A nasal mucosal flap is created and excised, after which the lacrimal bone is drilled with the use of a bone drilling device (Image 2).
This surgical technique has shown similar, and possibly even higher, success rates when compared to the older external approach, with the added advantage of sparing the pediatric patient a scar on the face
Featured in this article
Specialties & Programs
Nasolacrimal duct obstruction (NLDO) is common in the pediatric population. Lacrimal sac massages and/or antibiotic ointment are typically recommended for children under the age of 1. Dacryocystorhinostomy (DCR) is generally recommended for treatment of congenital NLDO when a prior probing with stent placement has failed, or in the setting of dacryocystitis (an infection of the lacrimal sac).
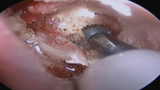
The surgical technique for DCR traditionally required a skin incision over the lacrimal sac. However, the newer technique does not and, as shown in the photos to the right, involves the use of an endoscopic camera to visualize the intranasal space. A light pipe is used to cannulate the proximal tear system and lacrimal sac via the upper or lower punctum, and this transilluminates through the nasal mucosa. With the help of direct endoscopic visualization in the nose, the area of the lacrimal sac fossa is identified as it illuminates (Image 1). A nasal mucosal flap is created and excised, after which the lacrimal bone is drilled with the use of a bone drilling device (Image 2).
This surgical technique has shown similar, and possibly even higher, success rates when compared to the older external approach, with the added advantage of sparing the pediatric patient a scar on the face
Contact us
Division of Ophthalmology