A 14-year-old female presents for a routine sports physical. She is a long-time patient of your practice and has been previously healthy, including normal growth and development and onset of menses at 12 years of age. Her height is at the 75th percentile and weight at the 65th percentile, both leveling off over the last 12 months. On exam you notice a mass in her anterior neck, midway between her chin and clavicles, about 1 cm off the midline to the left. The mass is about 1.5 cm in greatest dimension. On the same side, you palpate lymph nodes along the anterior edge as well as posterior to her sternocleidomastoid. The midline mass moves with swallowing and none of these lesions are painful. You do not feel any mass on the right, however; you palpate several smaller lymph nodes under the angle of her jaw. The remainder of her exam is normal.
The family is surprised by your findings. On more directed questioning she is asymptomatic and denies weight loss, night sweats, hoarseness, and dysphagia. She has not traveled recently and has no new pets at home. There are no cancers with increased incidence in the family. Her last exam for an acute illness about 6 months ago did not document similar findings.
Discussion: The diagnosis is papillary thyroid carcinoma. PTC is one of two subtypes of differentiated thyroid cancer (DTC): PTC and follicular thyroid cancer (FTC), with PTC comprising 85% to 90% of cases. DTC most frequently occurs as a sporadic condition although there are increasing reports of familial DTC which may occur in isolation or be a part of a tumor syndrome, including familial adenomatous polyposis, PTEN hamartoma syndrome, pleuropulmonary blastoma DICER1 syndrome, and others. Familial DTC is defined by 2 or more first-degree relatives having the disease with an associated 8- to 10-fold increased risk for other first-degree relatives developing DTC compared to the general population.
PTC is most commonly diagnosed after the incidental discovery of an asymptomatic thyroid nodule either during physical exam or during non-thyroid related head and neck imaging. PTC may also present as persistent cervical lymphadenopathy and, thus, a thyroid ultrasound (US) should be considered as part of the evaluation of persistent adenopathy prior to proceeding with biopsy.
For unknown reasons, there are an increasing number of both pediatric and adult patients being diagnosed with thyroid nodules as well as thyroid cancer, with thyroid cancer now the second-most frequently diagnosed malignancy in Caucasian girls aged 15 to 19. Risk factors include previous exposure to ionizing radiation (most frequently associated with treatment of a non-thyroid malignancy), iodine deficiency, and autoimmune thyroiditis.
When thyroid nodules are discovered in pediatric patients, there is a 5-fold higher risk of malignancy when compared to adults, approximately 25% to 30% vs. 5% to 10%, respectively. However, based on these estimates, the majority are benign; the challenge is to determine which patients warrant further evaluation and treatment. As with all diagnoses, a thorough history and physical exam are essential, focusing on review of known risk factors (discussed above) and documentation of the location and texture of the nodule(s) as well as any abnormal cervical lymph nodes. A thyroid and neck ultrasound provides further characterization of the nodule(s) and lymph nodes (See Figure 1). Based on these data, patients are then stratified to either undergo fine needle aspiration (FNA) biopsy or to continue clinical surveillance. The use of conscious sedation, US guidance, bedside confirmation of sample adequacy, and review by a cytopathologist with extensive experience in evaluating thyroid disease is essential for an accurate FNA diagnosis.
Figure 1: Ultrasound Images of the Thyroid and Cervical Lymph Nodes
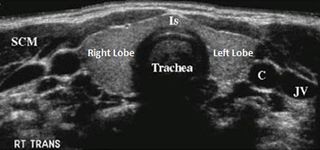
A normal appearing thyroid gland (Is: isthmus) with adjacent structures (SCM: sternocleidomastoid muscle, C: carotid artery, JV: jugular vein)

A complex, mostly cystic thyroid nodule in the right thyroid lobe. These complex nodules have a lower risk of malignancy.
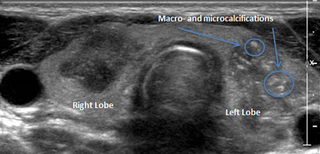
Two large, hypoechoic nodules associated with poorly defined borders, the left-sided nodules showing macro- and microcalcifications.
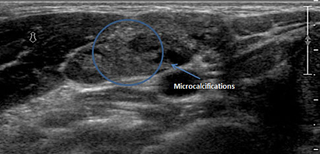
An abnormal lymph node, round in shape with microcalcifications (shown) and increased peripheral blood flow (not shown). These features are very consistent with thyroid metastasis.
With appropriate evaluation and management, the prognosis of DTC in children and adolescents is excellent. This is true even for patients who present with local or distant metastases, which occur in 50% to 60% and 15% to 20%, respectively. Unfortunately, while disease-specific mortality is low, disease-specific morbidity is relatively high secondary to complications of surgery and therapy. These risks can be significantly reduced if patients are evaluated and cared for in a center organized, resourced, and experienced in managing patients with thyroid disease, including thyroid nodules and thyroid cancer. Access to a surgeon who performs more than 30 thyroid surgeries per year is the most important initial step in increasing the likelihood of good outcome. The selective use of radioiodine therapy is also a critical aspect of care. Long-term follow-up is essential, as up to 30% of patients experience recurrence over 3 to 4 decades of follow-up.
Our patient had a total thyroidectomy with central neck lymph node dissection. Post-operative staging revealed a small focus of uptake in the central neck that was treated with radioiodine therapy. She is currently back to her usual routine, on TSH-suppressive therapy, and being followed on an every 3-month surveillance plan. With continued care, she will have no limitations and will experience excellent long-term prognosis.
Referral Information
To refer a patient, call 215-590-3174. For information on thyroid nodules and thyroid cancer, visit the Pediatric Thyroid Center.
Online Figure 1: Functional Imaging
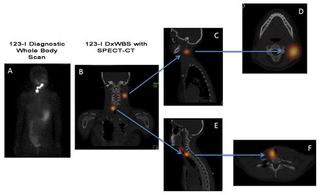
Functional imaging allowing for greater delineation of anatomic location of persistent, metastatic thyroid cancer: 123-I diagnostic whole body scan (DxWBS) showing uptake in the central and lateral neck. The addition of SPECT-CT (single photon emission CT; images B-> F) to the 123-I scan provides exact anatomic location of the uptake allowing for improved surgical planning.
A 14-year-old female presents for a routine sports physical. She is a long-time patient of your practice and has been previously healthy, including normal growth and development and onset of menses at 12 years of age. Her height is at the 75th percentile and weight at the 65th percentile, both leveling off over the last 12 months. On exam you notice a mass in her anterior neck, midway between her chin and clavicles, about 1 cm off the midline to the left. The mass is about 1.5 cm in greatest dimension. On the same side, you palpate lymph nodes along the anterior edge as well as posterior to her sternocleidomastoid. The midline mass moves with swallowing and none of these lesions are painful. You do not feel any mass on the right, however; you palpate several smaller lymph nodes under the angle of her jaw. The remainder of her exam is normal.
The family is surprised by your findings. On more directed questioning she is asymptomatic and denies weight loss, night sweats, hoarseness, and dysphagia. She has not traveled recently and has no new pets at home. There are no cancers with increased incidence in the family. Her last exam for an acute illness about 6 months ago did not document similar findings.
Discussion: The diagnosis is papillary thyroid carcinoma. PTC is one of two subtypes of differentiated thyroid cancer (DTC): PTC and follicular thyroid cancer (FTC), with PTC comprising 85% to 90% of cases. DTC most frequently occurs as a sporadic condition although there are increasing reports of familial DTC which may occur in isolation or be a part of a tumor syndrome, including familial adenomatous polyposis, PTEN hamartoma syndrome, pleuropulmonary blastoma DICER1 syndrome, and others. Familial DTC is defined by 2 or more first-degree relatives having the disease with an associated 8- to 10-fold increased risk for other first-degree relatives developing DTC compared to the general population.
PTC is most commonly diagnosed after the incidental discovery of an asymptomatic thyroid nodule either during physical exam or during non-thyroid related head and neck imaging. PTC may also present as persistent cervical lymphadenopathy and, thus, a thyroid ultrasound (US) should be considered as part of the evaluation of persistent adenopathy prior to proceeding with biopsy.
For unknown reasons, there are an increasing number of both pediatric and adult patients being diagnosed with thyroid nodules as well as thyroid cancer, with thyroid cancer now the second-most frequently diagnosed malignancy in Caucasian girls aged 15 to 19. Risk factors include previous exposure to ionizing radiation (most frequently associated with treatment of a non-thyroid malignancy), iodine deficiency, and autoimmune thyroiditis.
When thyroid nodules are discovered in pediatric patients, there is a 5-fold higher risk of malignancy when compared to adults, approximately 25% to 30% vs. 5% to 10%, respectively. However, based on these estimates, the majority are benign; the challenge is to determine which patients warrant further evaluation and treatment. As with all diagnoses, a thorough history and physical exam are essential, focusing on review of known risk factors (discussed above) and documentation of the location and texture of the nodule(s) as well as any abnormal cervical lymph nodes. A thyroid and neck ultrasound provides further characterization of the nodule(s) and lymph nodes (See Figure 1). Based on these data, patients are then stratified to either undergo fine needle aspiration (FNA) biopsy or to continue clinical surveillance. The use of conscious sedation, US guidance, bedside confirmation of sample adequacy, and review by a cytopathologist with extensive experience in evaluating thyroid disease is essential for an accurate FNA diagnosis.
Figure 1: Ultrasound Images of the Thyroid and Cervical Lymph Nodes
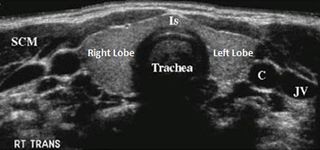
A normal appearing thyroid gland (Is: isthmus) with adjacent structures (SCM: sternocleidomastoid muscle, C: carotid artery, JV: jugular vein)

A complex, mostly cystic thyroid nodule in the right thyroid lobe. These complex nodules have a lower risk of malignancy.
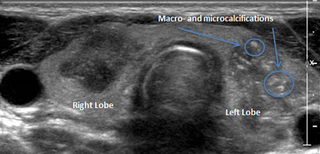
Two large, hypoechoic nodules associated with poorly defined borders, the left-sided nodules showing macro- and microcalcifications.
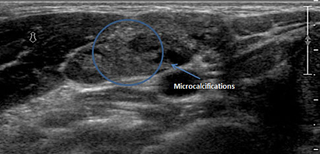
An abnormal lymph node, round in shape with microcalcifications (shown) and increased peripheral blood flow (not shown). These features are very consistent with thyroid metastasis.
With appropriate evaluation and management, the prognosis of DTC in children and adolescents is excellent. This is true even for patients who present with local or distant metastases, which occur in 50% to 60% and 15% to 20%, respectively. Unfortunately, while disease-specific mortality is low, disease-specific morbidity is relatively high secondary to complications of surgery and therapy. These risks can be significantly reduced if patients are evaluated and cared for in a center organized, resourced, and experienced in managing patients with thyroid disease, including thyroid nodules and thyroid cancer. Access to a surgeon who performs more than 30 thyroid surgeries per year is the most important initial step in increasing the likelihood of good outcome. The selective use of radioiodine therapy is also a critical aspect of care. Long-term follow-up is essential, as up to 30% of patients experience recurrence over 3 to 4 decades of follow-up.
Our patient had a total thyroidectomy with central neck lymph node dissection. Post-operative staging revealed a small focus of uptake in the central neck that was treated with radioiodine therapy. She is currently back to her usual routine, on TSH-suppressive therapy, and being followed on an every 3-month surveillance plan. With continued care, she will have no limitations and will experience excellent long-term prognosis.
Referral Information
To refer a patient, call 215-590-3174. For information on thyroid nodules and thyroid cancer, visit the Pediatric Thyroid Center.
Online Figure 1: Functional Imaging
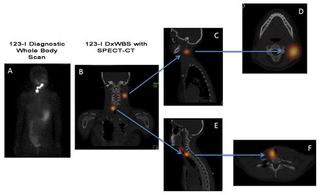
Functional imaging allowing for greater delineation of anatomic location of persistent, metastatic thyroid cancer: 123-I diagnostic whole body scan (DxWBS) showing uptake in the central and lateral neck. The addition of SPECT-CT (single photon emission CT; images B-> F) to the 123-I scan provides exact anatomic location of the uptake allowing for improved surgical planning.