Fine Needle Aspiration
What is fine needle aspiration?
A thyroid fine needle aspiration (FNA) is a procedure used to determine whether a thyroid nodule is more likely to be cancerous or benign (not a cancer). During FNA, an interventional radiologist uses a very thin needle — skinnier than the needle used for blood draws — to extract a sample of cells from a thyroid nodule and/or lymph node.
Not all thyroid nodules require FNA. Children with thyroid nodules are first assessed with a thyroid and neck ultrasound. The ultrasound images are reviewed in detail by a radiologist to determine if the thyroid nodule has concerning characteristics and to look for abnormal lymph nodes in the neck.
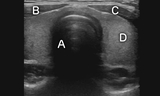
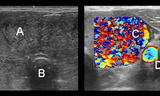
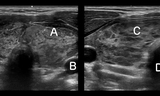
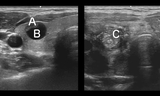
Thyroid Ultrasound images
At the Pediatric Thyroid Center at Children’s Hospital of Philadelphia (CHOP), additional ultrasound images are obtained using point-of-care (POC) ultrasound, an ultrasound exam that is performed during the clinic visit. The use of POC ultrasound enables the endocrinologist to review images with the patient and family while providing complete, direct and real-time assessment. POC ultrasound also helps to ensure efficient and accurate decision-making if the initial images do not provide complete information to determine whether a nodule should undergo FNA or surveillance. CHOP is one of few pediatric thyroid clinics in the United States with the ability to perform POC ultrasound.
If FNA is indicated, our experts will thoroughly explain the process and potential outcomes prior to referral to Interventional Radiology, where the procedure is performed.
What happens during fine needle aspiration?
CHOP’s Pediatric Thyroid Center has refined the techniques and streamlined the process needed to perform FNA for children and adolescents. All patients are offered moderate sedation to optimize comfort, decrease anxiety and ensure an adequate sample is obtained. An interventional radiologist first performs an additional ultrasound to confirm the location and appearance of all thyroid nodules and lymph nodes. The selected thyroid nodules and/or lymph nodes then undergo FNA.
FNA is performed with ultrasound guidance to ensure safe and accurate sampling. An entry site for the needle is chosen, and a small amount of local anesthetic is injected to numb the skin. The thin needle is carefully advanced into the nodule, manipulated to acquire the cells, and then removed. Each nodule may need to be sampled a few times. Overall, the FNA procedure takes approximately 1 to 2 hours, with the majority of time spent preparing for the procedure and recovering from sedation.
The doctors who interpret the results of FNA are called cytopathologists. Accurate interpretation is critical to making the best decision for each patient. CHOP partners with the Hospital of the University of Pennsylvania (HUP), where the cytopathologists are world-renowned for evaluating thyroid cells. We are one of few pediatric thyroid centers in the country where a cytophathologist is present during FNA. The cytopathologist reviews the sampled cells to ensure an adequate sample is obtained and to provide a preliminary interpretation of the result.
For samples with indeterminate cells (cells that are not clearly benign or cancerous), an additional sample from the nodule is obtained during the procedure for oncogene testing. This genetic test can provide additional information and help determine if surgery (and what extent of surgery) is needed.
The final results of the FNA, provided by the cytopathologist a few days after the procedure, will be used to guide further management.
The system used to report results is called The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC), a six-tiered scoring system. When FNA is considered, your provider will review with you the potential results of FNA based on TBSRTC.
Does fine needle aspiration hurt?
FNA is not a painful procedure. Numbing medicine at the skin helps keep children comfortable. All CHOP patients are also offered sedation prior to the procedure for added comfort and to reduce anxiety.
Most patients who remain awake for the procedure report feeling pressure as the sample is obtained. After the procedure, a Band-Aid is often placed at the site. Unlike surgical thyroid biopsy, FNA is minimally invasive and does not scar; however, the needle may leave a small bruise, and some patients report mild soreness for 1-2 days after the procedure.
How soon will I receive the results of fine needle aspiration?
Official results are typically available in 5 to 7 days. When the FNA is scheduled, the Thyroid Center team will call to arrange a follow-up appointment. Your team may also call you with the results prior to your follow-up appointment.
Can fine needle aspiration be used to treat thyroid nodules?
Certain thyroid nodules may be treated by FNA technique. These include fluid-filled nodules, called thyroid cysts. In the case of thyroid cysts, the fluid is removed using FNA. Then sterile, medical-grade alcohol called ethanol is injected into the cyst. The ethanol is allowed to sit for a short period of time and is then removed. The ethanol irritates the lining of the cyst, decreasing the chance for fluid to reaccumulate. This procedure is called sclerotherapy.
Injection of ethanol by fine needle may also be used to destroy small lymph nodes (usually less than 1 centimeter) with metastatic papillary thyroid cancer.This procedure is called ultrasound-guided percutaneous ethanol ablation (PEA). In PEA, the ethanol volume is even smaller, and it is left in the lymph node after injection. The goal of PEA is to destroy the lymph node without additional surgery or radioactive iodine. For most patients, PEA involves two or more injections, usually 6 to 12 months apart. Your Thyroid Center provider and interventional radiologist will discuss these procedures with you if they feel your child would be a good candidate.