Responsive Neurostimulation for Epilepsy: AJ’s Story
Responsive Neurostimulation for Epilepsy: AJ’s Story
AJ’s life was relatively uncomplicated until age 14, when he began to experience unpredictable seizures and received a life-changing diagnosis of epilepsy. Thanks to the combination of a small, battery-powered device surgically implanted into his brain and an oral medication, he is now seizure-free.

AJ's first seizure happened on a family trip to Boise, Idaho. He was on a moving walkway in the Salt Lake City airport and started to have an aura. When he got to the end of the walkway, he dropped his bags, fell to the ground and had a seizure; his left arm hovered over his chest and he stared blankly into the distance. The seizure lasted about a minute.
His parents took him to a physician in Boise who diagnosed AJ with epilepsy and prescribed him anti-seizure medication. AJ had two more seizures on the trip. When the family got back to their home in Phillipsburg, NJ, they took AJ to a nearby neurologist who prescribed a second medication.
Even with two medications, the seizures continued. They came in one of two forms: either a mild seizure that lasted about 45 seconds and that AJ recovered from quickly, or a harsher, convulsive seizure that lasted two to three minutes and involved his whole body. For the longer seizures, AJ would black out and have no memory of the episode. Afterward, he would be wiped out, feel ill and sleep for hours. His only warning that a seizure was coming was an aura about 10 seconds in advance. Some people’s auras take the form of flashing lights or zigzag lines; in AJ’s case, it was an unusual sensation.
Seeking specialized epilepsy care
AJ’s mom, Teri, did some research online and came across the Pediatric Epilepsy Program at Children’s Hospital of Philadelphia (CHOP), which is about a 1½ hour from Phillipsburg. The program is an accredited level 4 epilepsy center that specializes in the diagnosis, evaluation and treatment of children and adolescents with seizures and epilepsy.
Teri reached out to the program coordinator and made an appointment for AJ to undergo a comprehensive evaluation. Diagnostic tests determined that part of AJ’s brain hadn’t developed correctly from birth. Marissa Di Giovine, MD, AJ’s neurologist and Director of CHOP’s Responsive Neurostimulation Clinic, and other members of his care team were shocked that AJ had lived so long without having a seizure and at how functional he was.
“One wouldn’t realize the extent of his condition by merely looking at him or speaking to him,” says Dr. Di Giovine. “He is an exceptionally intelligent young man both academically and emotionally, and physically, he is quite athletic.”
Dr. Di Giovine modified AJ’s medications, but the seizures continued. Despite that, he always maintained a positive attitude and tried to live his life like a normal kid.
“Even if he had a setback because of a seizure, the way he would react to it was amazing,” says Teri. “He never let this change anything in his life. He’s never felt sorry for himself or been depressed about it. That’s just his personality.”
StereoEEG to pinpoint seizure location
When seizures don’t respond to medication, in some cases, the epilepsy team at CHOP considers surgery to remove the part of the brain causing the seizures, provided it isn’t too close to brain tissue that controls critical functions. Children who undergo the surgery can become seizure-free or have significantly fewer or less severe seizures.
First, the team needed to identify the point or points in the brain where AJ’s seizures originated. AJ would need to undergo stereoelectroencephalography (also known as sEEG or stereoEEG), a minimally invasive surgical procedure in which electrodes would be implanted directly into his brain around the area his physicians thought was causing his seizures. Benjamin Kennedy, MD, Director of Epilepsy and Functional Neurosurgery at CHOP, and his team in the Neurosurgery lab at CHOP are doing research to understand epileptic networks electrically using sEEG, as well as explain the genetic mechanisms of brain malformations, with the goal of developing more effective therapies for patients like AJ.
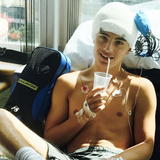
AJ was taken off his medications and spent 19 days in the hospital. During that time, his doctors monitored his seizures to see where exactly they were coming from. Understandably, the idea of brain surgery can be a scary thing for families, but sEEG is well tolerated by children of all ages. Dr. Di Giovine says AJ came out of neurosurgery smiling and gave her a thumbs-up.
“He approached the whole situation with more grace, bravery and humor than I could have ever hoped for with any of my patients,” says Dr. Di Giovine.
The procedure found AJ’s seizures originated from a large area on the right side of his brain that was very close to the area of the brain that controls hand sensation and movement. The team was concerned that removing the abnormal part of AJ’s brain would affect his ability to move his hand. Dr. Di Giovine told the family about a brand-new treatment that offered a better option for AJ.
Responsive neurostimulation to control seizures
Responsive neurostimulation (RNS) is a cutting-edge treatment for seizures in which a small, battery-powered device is surgically implanted into the skull with electrodes leading to points within the abnormal part of the brain where seizure activity is originating. When the electrodes sense abnormal brain activity, they emit mild electrical pulses that prevent or shorten the seizure. A piece of the skull is removed so the neurostimulator is flush with the outer surface of the skull, and it is put in a place where it is hardly noticeable in a child’s hair.
Because RNS is an advanced, precise procedure, it should be performed in a hospital with expert pediatric neurosurgeons and neurologists who have experience caring for children before during and after RNS surgery. Dr. Kennedy implanted the device in AJ’s brain when he was 18. He was the first pediatric patient at CHOP to undergo the procedure.
Shortly after the procedure, AJ and his family moved to Colorado, and AJ transitioned to an adult neurologist in Colorado. He returned to the East Coast in 2019 to speak at the American Epilepsy Society Meeting in Baltimore regarding his “transition of care” from pediatric neurology to adult neurology care.
Success with RNS and medication

With the RNS device, AJ’s seizure frequency decreased 50%. He had follow-up appointments every three months with his adult neurologist. In between appointments, AJ kept diligent records about his seizures. Every day, he used a remote monitor to collect data from the neurostimulator and uploaded the data to a secure web database. Then, at follow-up appointments, his neurologist adjusted the neurotransmitter to improve its detection of seizures and further reduce the seizure activity in AJ’s brain.
With each adjustment of the neurotransmitter, AJ saw an improvement. But he continued to average about one seizure a month. He tried to stay positive, but not knowing when or where he might have a seizure was a constant source of worry. As soon as he got an aura, he’d quickly find a safe place where he wouldn’t hit his head. Living with that fear prevented him from getting a driver’s license and even going swimming.
AJ’s neurologist was encouraged by the success an oral epilepsy medication showed in clinical trials. With the medication approved by the FDA to control partial-onset seizures in adults, he prescribed it to AJ. AJ began taking the medication in January 2022, and he hasn’t experienced a seizure since.
With this new medication plus the added protection from the RNS device, AJ has now experienced six months of complete seizure freedom. His neurologist decreased follow-up appointments to every six months.
Driving toward a brighter future

AJ, now 23, feels safer and finally able to let his guard down a bit. He finally felt confident enough to get his driver’s license.
“Having a driver’s license has given AJ more freedom, more confidence and more independence,” says his mom.
“I love it,” says AJ of his newfound independence.
In November 2022, he shared his story as part of CHOP’s family-focused epilepsy education series.
“I am so proud of AJ and the man he has become,” says Dr. Di Giovine. “He was a trailblazer.”