What is Hirschsprung’s disease?
Hirschsprung’s disease is a birth defect of the intestines in which nerves in the wall of the intestine do not form properly. Children with Hirschsprung’s disease are unable to defecate or pass stool, which can cause bowel obstruction. It can be life threatening if left untreated.
During normal fetal development, nerves called ganglion cells form in the intestinal walls along the entire digestive tract. These nerves trigger muscles in the intestine to squeeze and relax to move digested food through the intestines. This movement, called peristalsis, results in defecation (pooping). Without ganglion cells, the bowel does not relax and causes stool to build up in the intestine, which can result in a bowel obstruction.
Newborns with Hirschsprung’s disease will often have abdominal distension (an enlarged abdomen), while older children may suffer from chronic constipation.
Hirschsprung’s disease is rare, occurring in an estimated 1 in 5,000 births. It is more common in males than in females. Hirschsprung’s disease may also be called congenital megacolon or aganglionic megacolon.
Watch the video to learn more about our coordinated approach to caring for children with Hirschsprung's disease.
Symptoms of Hirschsprung’s disease
Hirschsprung’s disease is most often diagnosed in the newborn period within the first six weeks of life. Symptoms may include:
- Failure to pass stool within 24-48 hours after birth
- Poor appetite
- Vomiting
- Distended abdomen
Although much less common, older children can be diagnosed with Hirschsprung’s disease. Symptoms in older children with Hirschsprung’s disease may include:
- Poor appetite
- Distended abdomen
- Severe constipation
- Vomiting
- Poor growth
- Poor weight gain
Some infants and children present with Hirschsprung-associated enterocolitis, which is a life-threatening infection of the intestine seen in children with Hirschsprung’s disease. Signs and symptoms of enterocolitis are diarrhea, fever, abdominal distension and decreased energy. These signs and symptoms are considered serious and life-threatening. If they occur, notify your child's doctor immediately.
Diagnosis of Hirschsprung's disease
A careful physical examination and history are required to see if Hirschsprung’s disease is a possible diagnosis. Confirming a diagnosis may include any of the following studies:
- Abdominal X-ray shows if the intestine is abnormally large (dilated) above a blockage.
- Contrast enema provides more detail on the size of the intestine and rectum. A doctor will put barium (a chalky X-ray dye that coats the intestine) or water-soluble contrast (X-ray dye) into the rectum and intestine through a tube in the anus. The doctor will take X-rays to see if the intestine is dilated and if there is an area where the size changes significantly. This procedure can be performed in the Radiology Department at CHOP. It is not painful, and no sedation is required.
- Manometry is another way to determine if your child has Hirschsprung’s disease by testing the refluxes in the anus and rectum. A doctor will place a small balloon catheter (tube) in the anus and rectum to measure pressure changes and muscle movements. If there is normal pressure and movement, the child probably does not have Hirschsprung’s disease, and the doctor will not have to perform more invasive diagnostic tests such as biopsies. Manometry does not require anesthesia or sedation.
- Suction rectal biopsy involves taking a small sample of the lining of the intestine. This test is performed to provide a more definitive diagnosis if the X-ray and contrast enema suggest Hirschsprung’s disease in an infant. A surgeon will place an instrument through the anus into the rectum and take tiny pieces of the intestinal mucosa (moist tissue that lines the intestines). The tissue samples will be examined under a microscope. If ganglion cells are not present, doctors will know for sure that the child has Hirschsprung’s disease. This procedure can be performed at the bedside, if your child is an inpatient, or it can be performed in the surgeon’s office. It is not painful, and no sedation is required.
- Full-thickness biopsy is performed if the suction rectal biopsy results are inconclusive or if your child is older. The patient will be placed under general anesthesia and the surgeon will take a thicker piece of intestinal tissue. The tissue sample will be examined under a microscope. This can be done for diagnosis or for planning before surgical treatments, so the doctor can determine where the ganglion cells stop in the intestine.
Hirschsprung’s disease treatment
Definitive treatment for Hirschsprung’s disease is the surgical removal of the portion of the bowel without ganglion cells. Surgical correction may take up to three stages.
Children’s Hospital of Philadelphia has a special team of doctors and nurses who will help you manage this disorder before, during and after surgery so your child can remain as healthy as possible. Treatment for Hirschsprung’s disease varies based on each child’s symptoms and overall health. Your child’s treatment plan may include one or several of the following steps.
Please note that this information is meant to give an overview of possible treatments. Your child’s care team will work closely with your family to come up with the best recommended treatment plan for your child.
Rectal irrigation
Rectal irrigation is used to help your child defecate. A soft catheter (tube) is inserted through the anus into the rectum and the doctor flushes the rectum and intestine with saline solution in order to remove stool. This can be performed at the bedside. This may be used until surgery is performed and sometimes as a treatment afterward.
Leveling ostomy
Depending on the overall health of your child, a surgeon may decide they need a stoma — a surgically created opening in the bowel, also called an ostomy. The surgeon creates a small hole in the abdomen and brings a small portion of the intestine up to the skin. This allows stool to come out easily into a small bag.
For most children, the ostomy will be temporary with the goal of returning bowel function and allowing your child to eat and continue to grow before surgery.
Pull-through procedure for Hirschsprung's disease
In a pull-through procedure, a surgeon removes the abnormal section of the intestine and connects (“pulls through”) the healthy intestine with ganglion cells to replace it and connect to the rectum just above the anal sphincter.
After the pull-through procedure, your child will be able to go home when they are eating well, are passing stool and have no fever. Initially, your child will poop frequently. It is important to protect their skin with barrier creams. We will train you in this care. A small number of patients develop a leak, abscess or infection at the suture line (inside the anus).
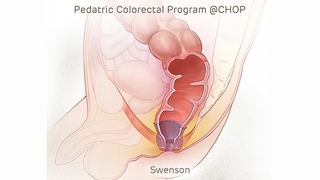
Image: The goal of all pull-through procedures is to bypass or remove the disease segment, as illustrated above using the Swenson technique.
If your child develops fever, abdominal distension (enlarged abdomen) or decreased stool output (is not pooping very much) we need to hear from you right away. Please call us at 215-590-2730.
Follow-up care for children with Hirschsprung’s disease
After your child undergoes a procedure, they will return for a follow-up appointment with their surgeon. After a pull-through procedure or ostomy closure procedure, children with Hirschsprung’s disease may continue to have some problems, which can include any of the following:
- Constipation — A high-fiber diet and fiber supplements can help prevent or minimize constipation.
- Bowel obstruction — This occurs when there is a blockage in the intestine. This may be due to a large amount of stool in the intestine, or it may be due to scar tissue after surgery. Signs and symptoms of a bowel obstruction include vomiting, pain and abdominal distension. Your child needs to be treated quickly if these symptoms occur.
- Severe diaper rash — After the pull-through procedure and colostomy closure (if performed), your child will experience frequent stooling resulting in many diaper changes. This can lead to significant diaper rash. The team will review with you techniques and products to help.
The Pediatric Colorectal Program will continue to follow your child’s progress closely after surgery. Your initial appointment following surgery will occur about two weeks after discharge and then monthly as directed by your surgeon. If your child continues to experience problems with bowel function or fecal incontinence, we will work with them on a long-term bowel management program and supplemental treatment that may include medications or a therapeutic diet.
Life-threatening complications related to Hirschsprung’s disease
Children with Hirschsprung’s disease are at risk for a serious condition called Hirschsprung’s enterocolitis. Enterocolitis is an inflammation in the lining of the intestinal wall that must be treated immediately. If left untreated, it can be life threatening. Enterocolitis can occur in children with ostomies, as well as children who have had a pull-through procedure.
If your child has any of the following symptoms, call us right away or take your child to an emergency room:
- Explosive diarrhea
- Unusually foul-smelling diarrhea
- Gray or pale-colored stool
- Vomiting
- Abdominal distension (swollen stomach area)
- Fever (with any of the other symptoms listed above)
- Lethargy (unusual sleepiness)
Why choose CHOP for Hirschsprung’s disease care
If your child is diagnosed with Hirschsprung’s disease and is suffering from stooling problems, Children’s Hospital of Philadelphia offers a wide variety of treatment options and every pediatric subspecialty your child may need in their care before, during and after surgery.
Our Pediatric Colorectal Program specializes in the evaluation, diagnosis, treatment and long-term management of children with colorectal conditions and anorectal continence issues such as Hirschsprung’s disease.
Your child will have access to expert pediatric colorectal surgeons, gastroenterologists, urologists and other specialists who understand the unique challenges faced by children with colorectal conditions and their families. We work together to manage the care of children with Hirschsprung’s disease and develop a personalized treatment plan for every patient.

Why choose CHOP
Learn more about our experience managing the care of children with bowel management needs and how our program can help.

Your child's appointment
Learn what to expect during your child's first appointment with CHOP’s Pediatric Colorectal Program.
Resources to help
Reviewed by Edward J. Doolin, MD, FACS, FAAP, Myron Allukian, III, MD


