Myelomeningocele (MMC) and myeloschisis (MS) are open spinal dysraphisms. In MMC, the neural placode extends through the spinal defect into a cerebrospinal fluid-filled meningeal sac, whereas in MS, an associated meningeal sac is absent and the cord remains within the spinal canal. In both disorders, leakage of cerebrospinal fluid (CSF) through the defect into the amniotic space has been hypothesized to result in loss of hydrostatic pressure in the spinal canal with consequent descent of the hindbrain through the foramen magnum. Loss of CSF results in a small posterior fossa and the classic Chiari II stigmata of downward displacement of the cerebellum and kinking of the brainstem.
Additional neurological damage results as the skin defect leaves neural tissue exposed and subject to mechanical trauma against the uterine wall and the neurotoxic effects of the amniotic fluid. The combined outcome of this abnormal developmental sequence culminates in lifelong disability with paralysis, incontinence and cognitive deficits.
The classic intracranial manifestations of open spinal dysraphisms can be demonstrated reliably by prenatal imaging studies and include the Chiari II malformation with a small posterior fossa, herniated cerebellar tonsils and ventriculomegaly. Talipes, or clubfoot deformity, and decreased lower-extremity motion are also sometimes present at the time of prenatal assessment, and lower extremity function is assessed routinely in cases of suspected spinal dysraphism.
We recently evaluated whether the presence of an MMC sac and sac size are associated with fetal talipes and abnormal lower-extremity function. We performed a search of a radiology database to identify cases of MMC and MS diagnosed prenatally at our Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment from 2013 to 2017. All cases were evaluated between 18 and 25 weeks. Ultrasound reports were reviewed for talipes and impaired lower-extremity motion. In MMC cases, sac volume was calculated from ultrasound measurements. Magnetic resonance imaging reports were reviewed for hindbrain herniation. The association of presence of an MMC sac and sac size with talipes and impaired lower-extremity motion was assessed. Post-hoc analysis of data from the multicenter Management of Myelomeningocele Study (MOMS) randomized controlled trial was performed to confirm the study findings.
What we found is that compared with MS cases, MMC cases with hindbrain herniation had a significantly higher rate of talipes or impaired lower-extremity movement. These findings — which were recently published in Ultrasound in Obstetrics & Gynecology — suggest that in fetuses with open spinal dysraphism, the risk of talipes is increased with an MMC sac, and that a larger sac may result in additional injury through mechanical stretching of the nerves.
A ‘two-hit’ hypothesis has been proposed to account for the final neurological outcome in open spinal dysraphism.
- Failure of neural tube closure represents the first ‘hit’
- Prolonged exposure of the neural elements to the intrauterine environment represents the second ‘hit’
The higher rate of prenatal talipes in MMC and the positive correlation between sac size and prenatal lower-extremity impairment suggest that additional neurological injury may occur through stretching of the neural placode and nerves from CSF hydrostatic forces within the MMC sac. This would represent a third acquired mechanism of injury (i.e., a ‘third hit’), adding to the mechanical injury from the uterine wall and amniotic fluid chemotoxicity experienced by the exposed spinal tissue. This damaging ‘stretch’ is not a factor in MS as no sac is present and the CSF streams out of the defect, unimpeded by a sac.
The presence of an MMC sac was associated with a significantly lower incidence of hindbrain herniation, which is similar to previous reports. These findings further support that MMC sac size may have a protective effect on the degree of hindbrain herniation by decreasing egress of CSF into the amniotic space and thereby maintaining some hydrostatic pressure within the spinal canal. Although the presence of a larger sac may exhibit a protective effect against hindbrain herniation, this paradoxically may increase the risk of talipes through increased traction of the neural placode and nerve roots.
The findings from this study may be of value in both prenatal counseling and pregnancy management, as they suggest that the fetal spinal cord and nerves are uniquely sensitive to stretch injury.
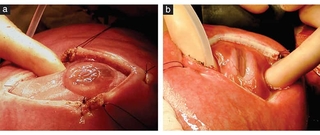
Image: Intraoperative photographs of myelomeningocele (MMC) (a) and myeloschisis (MS) (b) seen through hysterotomy during open fetal surgery. Neural placode and spinal nerves are stretched by distended sac in MMC case (a), whereas neural elements remain within canal in MS case (b).
Featured in this article
Specialties & Programs
Myelomeningocele (MMC) and myeloschisis (MS) are open spinal dysraphisms. In MMC, the neural placode extends through the spinal defect into a cerebrospinal fluid-filled meningeal sac, whereas in MS, an associated meningeal sac is absent and the cord remains within the spinal canal. In both disorders, leakage of cerebrospinal fluid (CSF) through the defect into the amniotic space has been hypothesized to result in loss of hydrostatic pressure in the spinal canal with consequent descent of the hindbrain through the foramen magnum. Loss of CSF results in a small posterior fossa and the classic Chiari II stigmata of downward displacement of the cerebellum and kinking of the brainstem.
Additional neurological damage results as the skin defect leaves neural tissue exposed and subject to mechanical trauma against the uterine wall and the neurotoxic effects of the amniotic fluid. The combined outcome of this abnormal developmental sequence culminates in lifelong disability with paralysis, incontinence and cognitive deficits.
The classic intracranial manifestations of open spinal dysraphisms can be demonstrated reliably by prenatal imaging studies and include the Chiari II malformation with a small posterior fossa, herniated cerebellar tonsils and ventriculomegaly. Talipes, or clubfoot deformity, and decreased lower-extremity motion are also sometimes present at the time of prenatal assessment, and lower extremity function is assessed routinely in cases of suspected spinal dysraphism.
We recently evaluated whether the presence of an MMC sac and sac size are associated with fetal talipes and abnormal lower-extremity function. We performed a search of a radiology database to identify cases of MMC and MS diagnosed prenatally at our Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment from 2013 to 2017. All cases were evaluated between 18 and 25 weeks. Ultrasound reports were reviewed for talipes and impaired lower-extremity motion. In MMC cases, sac volume was calculated from ultrasound measurements. Magnetic resonance imaging reports were reviewed for hindbrain herniation. The association of presence of an MMC sac and sac size with talipes and impaired lower-extremity motion was assessed. Post-hoc analysis of data from the multicenter Management of Myelomeningocele Study (MOMS) randomized controlled trial was performed to confirm the study findings.
What we found is that compared with MS cases, MMC cases with hindbrain herniation had a significantly higher rate of talipes or impaired lower-extremity movement. These findings — which were recently published in Ultrasound in Obstetrics & Gynecology — suggest that in fetuses with open spinal dysraphism, the risk of talipes is increased with an MMC sac, and that a larger sac may result in additional injury through mechanical stretching of the nerves.
A ‘two-hit’ hypothesis has been proposed to account for the final neurological outcome in open spinal dysraphism.
- Failure of neural tube closure represents the first ‘hit’
- Prolonged exposure of the neural elements to the intrauterine environment represents the second ‘hit’
The higher rate of prenatal talipes in MMC and the positive correlation between sac size and prenatal lower-extremity impairment suggest that additional neurological injury may occur through stretching of the neural placode and nerves from CSF hydrostatic forces within the MMC sac. This would represent a third acquired mechanism of injury (i.e., a ‘third hit’), adding to the mechanical injury from the uterine wall and amniotic fluid chemotoxicity experienced by the exposed spinal tissue. This damaging ‘stretch’ is not a factor in MS as no sac is present and the CSF streams out of the defect, unimpeded by a sac.
The presence of an MMC sac was associated with a significantly lower incidence of hindbrain herniation, which is similar to previous reports. These findings further support that MMC sac size may have a protective effect on the degree of hindbrain herniation by decreasing egress of CSF into the amniotic space and thereby maintaining some hydrostatic pressure within the spinal canal. Although the presence of a larger sac may exhibit a protective effect against hindbrain herniation, this paradoxically may increase the risk of talipes through increased traction of the neural placode and nerve roots.
The findings from this study may be of value in both prenatal counseling and pregnancy management, as they suggest that the fetal spinal cord and nerves are uniquely sensitive to stretch injury.
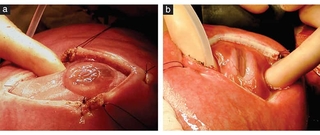
Image: Intraoperative photographs of myelomeningocele (MMC) (a) and myeloschisis (MS) (b) seen through hysterotomy during open fetal surgery. Neural placode and spinal nerves are stretched by distended sac in MMC case (a), whereas neural elements remain within canal in MS case (b).
Contact us
Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment