Case: A 15-year-old female presents with mild dyspnea with exertion, and frequent wet cough and throat-clearing. Her respiratory history is notable for asthma, 2 episodes of pneumonia and 2 episodes of influenza within the past year. A chest radiograph had shown a right middle lobe density during her second episode of pneumonia. She does not have a history of prematurity or chronic sinopulmonary infections, or symptoms of gastroesophageal reflux. She does not smoke tobacco products or use electronic cigarettes. There was no significant travel history or pets.
On physical exam, vital signs are normal. She has forced expiratory wheezes in both upper lobes, and no digital clubbing. A chest radiograph demonstrates mildly increased interstitial markings. Spirometry is normal, without significant bronchodilator response. Despite starting inhaled fluticasone (Flovent), a course of prednisone, and a 14-day course of amoxicillin-clavulanate to treat presumed protracted bacterial bronchitis, she has no improvement in symptoms and her dyspnea progressively worsens.
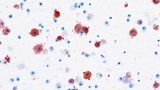
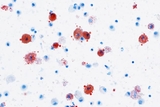
High resolution computed tomography (HRCT) of the chest is performed. Expiratory views show patchy areas of air trapping bilaterally. She undergoes flexible bronchoscopy with bronchoalveolar lavage (BAL). BAL findings are shown. (See Figure 1.)
Discussion: The diagnosis of lipoid pneumonia was made following referral to CHOP’s Division of Pulmonary and Sleep Medicine. The patient underwent a thorough step-wise workup, and ultimately the diagnosis was revealed by the bronchoalveolar lavage performed during bronchoscopy. The lipid-laden macrophages, along with extracellular lipid found on cytologic examination of the lavage fluid, suggested lipoid pneumonia. On further questioning, the patient and her mother supplied a long list of aerosolized and sprayed cosmetic and facial treatments, thus providing a source.
Lipoid pneumonia is a rare clinical entity wherein lipids accumulate in the lung. There are both endogenous and exogenous forms. The endogenous form includes processes in which lipids from within the lung itself accumulate, such as when alveolar cell walls are damaged and release lipid or when lipids builds up in lipid storage diseases. Exogenous lipoid pneumonia occurs from inhaled or aspirated lipid exposure, with cases reported due to aspiration of mineral oil as a treatment for constipation and excessive use of lip balm, petroleum jelly applied to the nares, among others. Typically, the process and presentation are chronic, although there have been cases of acute aspiration, such as “fire-eaters” who aspirate the flammable substance and develop symptoms within the first 12 hours.
Patients with lipoid pneumonia typically present with chronic cough, which may be dry or productive, and dyspnea. Patients can also report chest pain, hemoptysis, weight loss, and intermittent fever. Symptom severity has a wide range. Physical exam is similarly varied, and lung auscultation can be normal or reveal wheezes, crackles, or rhonchi. Without a history suggestive of exposure, presentation can be mistaken for asthma, protracted bacterial bronchitis, or atypical pneumonia. Failure of improvement with conventional therapies should prompt further investigation.
Chest radiograph can demonstrate abnormalities even in asymptomatic patients, although these findings are usually nonspecific. High-resolution chest computed tomography (HRCT) is the best imaging modality for establishing the diagnosis. The most specific finding on HRCT is lung consolidation with areas of fat attenuation. If the imaging is not definitive, BAL or lung biopsy (needle aspiration or open lung biopsy) can be helpful, as in this patient’s case. The exogenous lipid is taken up by macrophages, which are sampled by BAL. To obtain a BAL sample, a region of the lung is lavaged with a small amount of saline via bronchoscope, which can then be sent for microbiology and pathology studies.
Lipid-laden macrophages on BAL can be seen in several disorders, including both intrinsic and extrinsic processes. For example, this finding is seen in e-cigarette or vaping product use-associated lung injury (EVALI), which was included in the differential. In speaking frankly with the patient and her parents, she had denied electronic cigarette use, and parents did not report suspicions of use. Discussion of the case and the cytologic features of the BAL with our colleagues in the Department of Anatomic Pathology helped to narrow our focus to lipoid pneumonia. The discovery of extracellular lipid in the BAL pointed to lipoid pneumonia due to an exogenous source. Further history-taking revealed the likely causative agents to be the patient’s cosmetic sprays. Reviewing this list with the Poison Control Center at CHOP confirmed our suspicion that these products contained several possible lipid sources.
Withdrawal of the offending agent can lead to complete resolution, although in more severe cases, patients may develop long-term sequelae such as fibrosis and restrictive lung disease.
Patient update: Soon after discontinuation of cosmetic sprays, her symptoms resolved and she was able to resume her rigorous dance class schedule.
References and Selected Readings
Marchiori E, Zanetti G, Mano CM, Hochhegger B. Exogenous lipoid pneumonia. Clinical and radiological manifestations. Respir Med. 2011;105:659-666.
Betancourt SL, Martinez-Jimenez S, Rossi SE, Truong MT, Carrillo J, Erasmus JJ. Lipoid pneumonia: spectrum of clinical and radiologic manifestations. Am J Roentgenol. 2010;194:103-109.
Featured in this article
Specialties & Programs
Case: A 15-year-old female presents with mild dyspnea with exertion, and frequent wet cough and throat-clearing. Her respiratory history is notable for asthma, 2 episodes of pneumonia and 2 episodes of influenza within the past year. A chest radiograph had shown a right middle lobe density during her second episode of pneumonia. She does not have a history of prematurity or chronic sinopulmonary infections, or symptoms of gastroesophageal reflux. She does not smoke tobacco products or use electronic cigarettes. There was no significant travel history or pets.
On physical exam, vital signs are normal. She has forced expiratory wheezes in both upper lobes, and no digital clubbing. A chest radiograph demonstrates mildly increased interstitial markings. Spirometry is normal, without significant bronchodilator response. Despite starting inhaled fluticasone (Flovent), a course of prednisone, and a 14-day course of amoxicillin-clavulanate to treat presumed protracted bacterial bronchitis, she has no improvement in symptoms and her dyspnea progressively worsens.
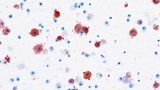
High resolution computed tomography (HRCT) of the chest is performed. Expiratory views show patchy areas of air trapping bilaterally. She undergoes flexible bronchoscopy with bronchoalveolar lavage (BAL). BAL findings are shown. (See Figure 1.)
Discussion: The diagnosis of lipoid pneumonia was made following referral to CHOP’s Division of Pulmonary and Sleep Medicine. The patient underwent a thorough step-wise workup, and ultimately the diagnosis was revealed by the bronchoalveolar lavage performed during bronchoscopy. The lipid-laden macrophages, along with extracellular lipid found on cytologic examination of the lavage fluid, suggested lipoid pneumonia. On further questioning, the patient and her mother supplied a long list of aerosolized and sprayed cosmetic and facial treatments, thus providing a source.
Lipoid pneumonia is a rare clinical entity wherein lipids accumulate in the lung. There are both endogenous and exogenous forms. The endogenous form includes processes in which lipids from within the lung itself accumulate, such as when alveolar cell walls are damaged and release lipid or when lipids builds up in lipid storage diseases. Exogenous lipoid pneumonia occurs from inhaled or aspirated lipid exposure, with cases reported due to aspiration of mineral oil as a treatment for constipation and excessive use of lip balm, petroleum jelly applied to the nares, among others. Typically, the process and presentation are chronic, although there have been cases of acute aspiration, such as “fire-eaters” who aspirate the flammable substance and develop symptoms within the first 12 hours.
Patients with lipoid pneumonia typically present with chronic cough, which may be dry or productive, and dyspnea. Patients can also report chest pain, hemoptysis, weight loss, and intermittent fever. Symptom severity has a wide range. Physical exam is similarly varied, and lung auscultation can be normal or reveal wheezes, crackles, or rhonchi. Without a history suggestive of exposure, presentation can be mistaken for asthma, protracted bacterial bronchitis, or atypical pneumonia. Failure of improvement with conventional therapies should prompt further investigation.
Chest radiograph can demonstrate abnormalities even in asymptomatic patients, although these findings are usually nonspecific. High-resolution chest computed tomography (HRCT) is the best imaging modality for establishing the diagnosis. The most specific finding on HRCT is lung consolidation with areas of fat attenuation. If the imaging is not definitive, BAL or lung biopsy (needle aspiration or open lung biopsy) can be helpful, as in this patient’s case. The exogenous lipid is taken up by macrophages, which are sampled by BAL. To obtain a BAL sample, a region of the lung is lavaged with a small amount of saline via bronchoscope, which can then be sent for microbiology and pathology studies.
Lipid-laden macrophages on BAL can be seen in several disorders, including both intrinsic and extrinsic processes. For example, this finding is seen in e-cigarette or vaping product use-associated lung injury (EVALI), which was included in the differential. In speaking frankly with the patient and her parents, she had denied electronic cigarette use, and parents did not report suspicions of use. Discussion of the case and the cytologic features of the BAL with our colleagues in the Department of Anatomic Pathology helped to narrow our focus to lipoid pneumonia. The discovery of extracellular lipid in the BAL pointed to lipoid pneumonia due to an exogenous source. Further history-taking revealed the likely causative agents to be the patient’s cosmetic sprays. Reviewing this list with the Poison Control Center at CHOP confirmed our suspicion that these products contained several possible lipid sources.
Withdrawal of the offending agent can lead to complete resolution, although in more severe cases, patients may develop long-term sequelae such as fibrosis and restrictive lung disease.
Patient update: Soon after discontinuation of cosmetic sprays, her symptoms resolved and she was able to resume her rigorous dance class schedule.
References and Selected Readings
Marchiori E, Zanetti G, Mano CM, Hochhegger B. Exogenous lipoid pneumonia. Clinical and radiological manifestations. Respir Med. 2011;105:659-666.
Betancourt SL, Martinez-Jimenez S, Rossi SE, Truong MT, Carrillo J, Erasmus JJ. Lipoid pneumonia: spectrum of clinical and radiologic manifestations. Am J Roentgenol. 2010;194:103-109.
Contact us
Division of Pulmonary and Sleep Medicine