In the Division of Pulmonary and Sleep Medicine — despite being proud of the care we provide and our outcomes — we are never satisfied. We always strive to do better and are constantly on the lookout for areas ripe for improving.
Our rigorous continuous quality improvement program is the vehicle we use to drive improvement. Our clinicians receive support from CHOP’s Office Clinical Quality Improvement, as needed.
Below, we highlight several active QI projects:
Technology Dependence Center
Our Technology Dependence Center (TDC), led by Howard Panitch, MD, has grown remarkably, and now follows more than 800 patients. (See Figure 1.)
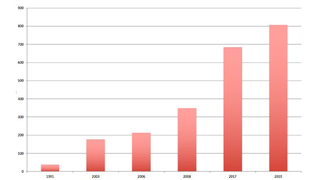
Figure 1: Growth of the Technology Dependence Program
In view of this nearly exponential growth, and in view of the importance of providing the right care in the right place for patients with complex respiratory disorders, the center has developed a transition program with the Division of Pulmonary and Sleep Medicine, Allergy and Critical Care at Penn Medicine. This will allow our patients, as they grow into adulthood, to smoothly transfer their care to adult care providers.
In addition, the TDC has conducted a CQI study to reduce the number of unanticipated rehospitalizations following initial discharge of ventilator-dependent children with tracheostomies, and another study to enhance caregivers’ adherence with carrying the appropriate supplies at all times for children with tracheostomies. The “Go Bag” contains suction, oxygen, additional tracheostomy tubes (the size used and one size smaller) and pulse oximeter, among other essential supplies.
Sleep Center
The Sleep Center has developed a QI initiative, under the direction of Suzanne Beck, MD, and psychologist Melissa Xanthopoulos, PhD, MS, focusing on CPAP adherence that has resulted in excellent outcomes. Approximately 140 infants and children are initiated on PAP each year and followed regularly by an interdisciplinary team of sleep doctors, respiratory therapists, behavioral psychologists, and sleep nurses. The QI project, showing improvement in both follow-up rate and timing of first titration PSG after CPAP start, was highlighted at the 2018 National SLEEP meetings in Baltimore. (See Figures 2 and 3.)
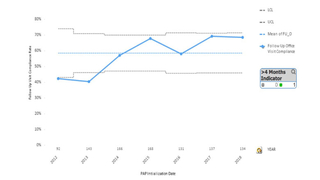
Figure 2: Follow up after CPAP Initiation
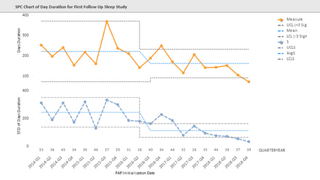
Figure 3: Time to titration/polysomnogram after CPAP initiation has improved since implementation of a QI Program in 2013. Mean time (orange line) and standard deviation (blue line) to first Titration/PSG after CPAP initiation shows a decrease over time reflecting implementation of a QI program in 2013 to track and coordinate care. After implementation the mean time to Titration/PSG as well as the standard deviation decreased due to tracking and coordinated care
Lung Transplant Center
The Lung Transplant Center has undertaken a comprehensive program to improve lung transplantation outcomes by a) monitoring immunosuppressive medications to ensure adequate drug levels while preventing toxicity and b) improving screening for opportunistic infections that could affect transplant outcomes.
The following transplant CQI projects yielded positive results:
- CMV screening: Interventions resulted in donor serology being entered in patient EHR 100% across all organ groups; smarttext being entered into EHR is increasing by 40%.
- Tacrolimus levels: Interventions increased percentage of tacrolimus troughs being drawn 11 to 13 hours after dose from 51% in 2017 to 67% in 2018.
- Pneumococcal vaccine: Interventions increased percentage from 64% in 2017 to 75% in 2018.
Asthma Program
Asthma quality improvement projects include improving how our respiratory therapists teach patients and families the proper technique for most effective use of inhalers and improving quality and consistency of spirometry across the CHOP Care Network. In addition, physicians are able to track and improve their performance in key elements of asthma care.
Featured in this article
Specialties & Programs
In the Division of Pulmonary and Sleep Medicine — despite being proud of the care we provide and our outcomes — we are never satisfied. We always strive to do better and are constantly on the lookout for areas ripe for improving.
Our rigorous continuous quality improvement program is the vehicle we use to drive improvement. Our clinicians receive support from CHOP’s Office Clinical Quality Improvement, as needed.
Below, we highlight several active QI projects:
Technology Dependence Center
Our Technology Dependence Center (TDC), led by Howard Panitch, MD, has grown remarkably, and now follows more than 800 patients. (See Figure 1.)
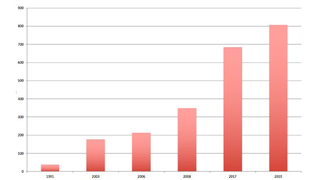
Figure 1: Growth of the Technology Dependence Program
In view of this nearly exponential growth, and in view of the importance of providing the right care in the right place for patients with complex respiratory disorders, the center has developed a transition program with the Division of Pulmonary and Sleep Medicine, Allergy and Critical Care at Penn Medicine. This will allow our patients, as they grow into adulthood, to smoothly transfer their care to adult care providers.
In addition, the TDC has conducted a CQI study to reduce the number of unanticipated rehospitalizations following initial discharge of ventilator-dependent children with tracheostomies, and another study to enhance caregivers’ adherence with carrying the appropriate supplies at all times for children with tracheostomies. The “Go Bag” contains suction, oxygen, additional tracheostomy tubes (the size used and one size smaller) and pulse oximeter, among other essential supplies.
Sleep Center
The Sleep Center has developed a QI initiative, under the direction of Suzanne Beck, MD, and psychologist Melissa Xanthopoulos, PhD, MS, focusing on CPAP adherence that has resulted in excellent outcomes. Approximately 140 infants and children are initiated on PAP each year and followed regularly by an interdisciplinary team of sleep doctors, respiratory therapists, behavioral psychologists, and sleep nurses. The QI project, showing improvement in both follow-up rate and timing of first titration PSG after CPAP start, was highlighted at the 2018 National SLEEP meetings in Baltimore. (See Figures 2 and 3.)
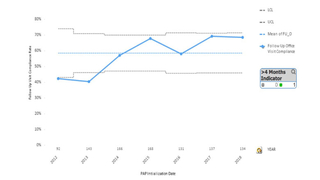
Figure 2: Follow up after CPAP Initiation
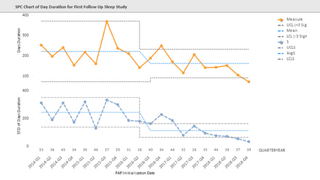
Figure 3: Time to titration/polysomnogram after CPAP initiation has improved since implementation of a QI Program in 2013. Mean time (orange line) and standard deviation (blue line) to first Titration/PSG after CPAP initiation shows a decrease over time reflecting implementation of a QI program in 2013 to track and coordinate care. After implementation the mean time to Titration/PSG as well as the standard deviation decreased due to tracking and coordinated care
Lung Transplant Center
The Lung Transplant Center has undertaken a comprehensive program to improve lung transplantation outcomes by a) monitoring immunosuppressive medications to ensure adequate drug levels while preventing toxicity and b) improving screening for opportunistic infections that could affect transplant outcomes.
The following transplant CQI projects yielded positive results:
- CMV screening: Interventions resulted in donor serology being entered in patient EHR 100% across all organ groups; smarttext being entered into EHR is increasing by 40%.
- Tacrolimus levels: Interventions increased percentage of tacrolimus troughs being drawn 11 to 13 hours after dose from 51% in 2017 to 67% in 2018.
- Pneumococcal vaccine: Interventions increased percentage from 64% in 2017 to 75% in 2018.
Asthma Program
Asthma quality improvement projects include improving how our respiratory therapists teach patients and families the proper technique for most effective use of inhalers and improving quality and consistency of spirometry across the CHOP Care Network. In addition, physicians are able to track and improve their performance in key elements of asthma care.
Contact us
Division of Pulmonary and Sleep Medicine