Staged Reconstruction Heart Surgery
To repair many types of single ventricle heart defects, including hypoplastic left heart syndrome (HLHS), tricuspid atresia, double outlet left ventricle (DOLV), some heterotaxy defects, and other congenital heart defects, surgeons often perform a series of open heart procedures over several years. This is called “staged reconstruction.” Surgeons reconfigure the heart and circulatory system during these procedures.
After the operations for single ventricle defects, the heart functions like a one-sided pump with two chambers. The heart no longer receives deoxygenated blood from the veins. Instead, this blood flows directly to the lungs. The heart receives oxygenated blood from the lungs and pumps it to the body. This is called Fontan circulation.
Stage 1: Norwood procedure
This operation will occur within several days of birth. Depending on the type of heart defect, different surgical procedures may be used, including the Norwood procedure. The purpose of this operation is to ensure that blood-flow is controlled enough to prevent damage to the heart and lungs, and that enough blood is reaching the lungs to keep the child alive until the second operation.

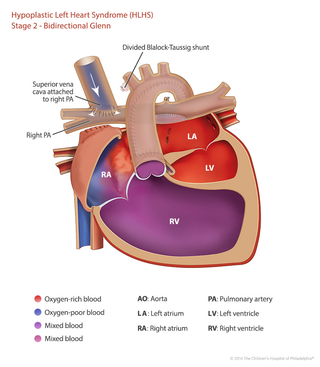
Stage 2: Hemi-Fontan or Glenn operation
Called the hemi-Fontan or Glenn operation, the second procedure usually occurs within six months of birth. During this surgery the superior vena cava — a large vein that carries deoxygenated blood from the upper body into the heart — is disconnected from the heart and attached to the pulmonary artery. After this operation, deoxygenated blood from the upper body goes to the lungs without passing through the heart.
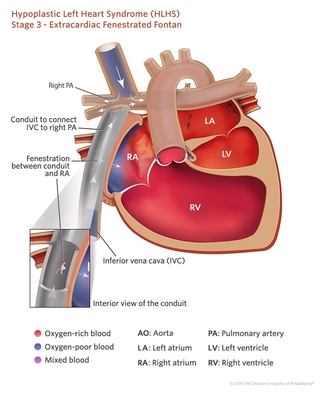
Stage 3: Fontan procedure
This operation, called the Fontan procedure, occurs at approximately 1 1/2 to 3 years of age. During this surgery the inferior vena cava, a large vein that carries deoxygenated blood from the lower body into the heart, is disconnected from the heart and attached to the pulmonary artery. After this operation, all of the deoxygenated blood from the body goes to the lungs without passing through the heart.
Frequent surveillance in infancy and early childhood is important to minimize risk factors for the eventual Fontan operation. The Infant Single Ventricle Monitoring Program at CHOP was developed to provide care and monitoring for children between the first two surgical procedures.
Your child will also need a customized series of diagnostic tests between the planned stages of surgery, and throughout childhood. Additional surgical or catheter therapies, or in rare cases heart transplantation, may also be recommended.