What is medullary thyroid cancer?
Medullary thyroid cancer (MTC) is a rare form of cancer that accounts for less than 2 percent of all thyroid cancers in the United States. MTC originates from the parafollicular C cells of the thyroid gland, which secrete the hormone calcitonin. The calcitonin hormone works together with the parathyroid hormone (a protein hormone secreted by parathyroid cells) to regulate calcium levels in the body.
Parafollicular C cells are different than follicular cells of the thyroid which are associated with differentiated thyroid cancer. The most important difference is that parafollicular C cells do not have the ability to absorb iodine, which can make treatment options more limited for children with recurrent or persistent medullary thyroid cancer.
Causes of medullary thyroid cancer
Medullary thyroid cancer is caused by a change or alteration in a specific gene called a RET proto-oncogene, which allows affected cells to grow and multiply rapidly, as well as function without any control or regulation.
The abnormal RET genes may occur spontaneously (called a de novo mutation) or may be passed from one generation to the next. The RET proto-oncogenes are inherited in an autosomal dominant pattern, meaning that if one parent has a specific RET gene, there is a 50 percent chance their child will inherit the same gene and develop medullary thyroid cancer.
In children, medullary thyroid cancer is often associated with multiple endocrine neoplasia, type 2 (MEN2), a rare inherited cancer syndrome. People with multiple endocrine neoplasia (MEN) develop tumors in the thyroid gland and other endocrine tissues. Depending on the specific mutations of the disorder — and which tissues are affected — MEN can be designated as type 1 or type 2. MEN1 is not associated with any form of thyroid cancer.
For patients with a gene mutation that leads to MEN2, there is a nearly 100 percent chance of developing medullary thyroid cancer. Because the RET protein is always active, cells receive signals to continuously multiply and contribute to cancer development. The timing of when the medullary thyroid cancer develops can be estimated based on the specific RET mutation and family history. The American Thyroid Association recently released guidelines that detail the known risk as moderate, high or highest for individuals with each gene mutation known to produce MTC.
Signs and symptoms of MTC
The symptoms associated with medullary thyroid cancer are similar to other forms of thyroid cancer such as differentiated thyroid cancer.
Symptoms may include:
- A visible lump (nodule)
- The sensation of a lump with swallowing
- Hoarseness or enlarged lymph nodes that do not go away
For patients with medullary thyroid cancer and MEN2 type B, additional physical features may be present. In infancy, the most common signs are the inability to make tears (alacrima) and constipation. In school-age children, symptoms include:
- An elongated face (marfanoid facies)
- Nodules on the lips, tongue or on the inside cheeks of the mouth (mucosal neuromas)
- Droopy or swollen-appearing eyelids or lips
- Scoliosis
- Constipation
School-age children with abdominal distension and constipation should also be evaluated for Hirschsprung’s disease, a rare intestinal disorder, which is often associated with MEN2 type A.
Testing and diagnosis of MTC
If there is any indication your child may have thyroid cancer, they should be referred to dedicated program, like the Pediatric Thyroid Center at CHOP, that has the experience, expertise and resources to fully evaluate your child.
At Children’s Hospital of Philadelphia, a diagnosis of medullary thyroid cancer begins with a complete medical history and comprehensive physical examination that includes evaluation of the thyroid and the lymph nodes in the neck. Watch CHOP Endocrinologist Andrew J. Bauer, MD, perform a pediatric thyroid exam.
Clinical experts may use a variety of diagnostic tests including:
- Blood test to measure the levels of calcitonin and thyroid-stimulating hormone (TSH) to determine how well your child’s thyroid is working.
- Thyroid ultrasound (or thyroid scan) to learn about the size, number, appearance and location of any thyroid nodules and abnormal lymph nodes.
- Fine-needle aspiration (FNA) to collect cells from the thyroid, and possibly lymph nodes, to be examined under a microscope.
Treatment for medullary thyroid cancer
Since medullary thyroid cancer originates from the parafollicular cells of the thyroid gland, and these cells do not absorb iodine, radioactive iodine (RAI) therapy is not an effective treatment to target tumor cells that have spread outside of the thyroid gland.
There are several other chemotherapy medications currently under investigation, but, for now, these medications only seem to slow down tumor growth. None appears to lead to a cure.
Surgery
The only effective treatment for medullary thyroid cancer is to surgically remove the entire thyroid gland, a procedure called a total thyroidectomy. For patients with an identified RET mutation, the goal of treatment is to remove the thyroid gland before medullary thyroid cancer develops and spreads.
After surgery, your child will remain in the Hospital for two to three days. This allows your child time to recover, ensure their pain is under control, and monitor for any potential side effects of surgery such as low calcium levels or RLN damage.
In most cases, surgical pain usually goes away within the first few days and most return to school within four to five days, and full activity within two weeks. The surgical scar is usually 3-4 centimeters in length and located in a skin fold to make it less noticeable. Absorbable sutures (stitches) and steri-strips are used so there is no need to have stitches removed.
Hormone replacement therapy
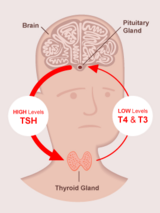
After a thyroidectomy, your child will no longer make thyroid hormone on their own. Your child will need to take thyroid hormone in order to get their thyroxine hormone (T4) and their thyroid-stimulating hormone (TSH) in normal ranges.
Thyroid hormone suppression
For patients with thyroid cancer, we prescribe higher doses of thyroid hormone replacement therapy with the goal of making the T4 high-normal or just above the normal limit, with the TSH below the normal limit. This is called suppressive therapy and is used because TSH can stimulate normal — as well as thyroid cancer cells — to grow. Using a suppressive therapy helps to decrease the risk that any remaining cancer cells will grow.
With the higher doses of thyroid hormone replacements, children may experience mild symptoms of hyperthyroidism, including:
- Anxiousness, irritability and/or nervousness
- Poor, restless sleep
- Increased activity (fidgetiness, hyperactivity, restlessness)
- Fatigue
- Increased appetite with or without weight loss
- Increased number of bowel movements per day
- Heat intolerance (always feeling warm)
- Decreased or poor school performance; difficulty concentrating that may be diagnosed as "late-onset" attention deficit disorder
If any of these symptoms are affecting your child’s daily activities, please contact your healthcare team to determine if the dose can be adjusted.
Follow-up care for MTC
Most children treated for medullary thyroid cancer will need long-term follow-up care into adulthood. In the first few years after surgery, your child will require physical exams and laboratory tests every three to six months.
As time passes — and if there is no evidence of recurrence — follow up exams may become yearly. Your child’s healthcare team will customize a follow-up plan based on your child’s condition and outcome.
After surgery and hormone replacement therapy many children will achieve remission, that is, they will have no clinical evidence, imaging evidence or evidence through laboratory testing of medullary thyroid cancer. However, others may develop persistent or recurrent thyroid cancer and the cancer may spread to other organs.
Persistent thyroid cancer is defined as evidence of disease by physical exam, laboratory testing and/or imaging six to 12 months after initial treatment. Recurrent thyroid disease is defined as a return of clinical disease after a patient was considered free of disease for six months or more.
Patients who develop persistent medullary thyroid cancer that does not respond to typical treatments will be referred to the Advanced Pediatric Thyroid Cancer Therapeutics Clinic, an innovative new collaborative program between Children’s Hospital of Philadelphia (CHOP) and the Hospital at the University of Pennsylvania (HUP). Under the guidance of Marcia S. Brose, MD, PhD, Director of the Thyroid Cancer Therapeutics Program at HUP, and Dr. Bauer, Director of the Pediatric Thyroid Center at CHOP, endocrinologists will determine which medications are likely to be most effective for your child, when specific medications should start and stop (sometimes in combinations), as well as the correct dosage based on your child’s age, weight and overall condition.
Outlook for medullary thyroid cancer
Patients who had their thyroid gland removed before medullary thyroid cancer developed have no risk for recurrence. For patients who were treated after medullary thyroid cancer developed, the chance of remission varies and is largely dependent on how extensively the cancer had spread. However, even in patients with extensive cancer spread, it may be years or even decades before the tumor continues to progress.
Resources to help
Medullary Thyroid Cancer Resources
Pediatric Thyroid Center Resources
We have created resources, including videos, to help you find answers to your questions and feel confident with the care you are providing your child.
