What is hyperthyroidism?
Hyperthyroidism (overactive thyroid) is a condition in which your child’s thyroid gland makes too much thyroid hormone. The over-secretion of thyroid hormone leads to over-activity of your child’s metabolism and can cause weight loss, a rapid or irregular heartbeat, sweating, nervousness, irritability, anxiety and decreased school performance.
Treatment for hyperthyroidism depends on the severity of your child’s condition. Most children are helped with anti-thyroid medications. Another treatment option is radioactive iodine to slow the production of thyroid hormone. In some cases, surgery to remove part or all of your child’s thyroid gland is necessary.
Types of hyperthyroidism
There are several types of hyperthyroidism. The most common are:
Graves' disease
Graves’ disease is much less common than autoimmune hypothyroidism (also known as Hashimoto’s thyroiditis). It is more common in girls than in boys, and more common in adolescents.
Hyperfunctioning thyroid nodules
Hyperfunctioning thyroid nodules are another form of hyperthyroidism. They occur when one or more benign growths in your child’s thyroid produce too much thyroid hormone. The majority of hyperfunctioning nodules are benign (not cancerous). However, fine needle aspiration is often performed to confirm the nodule is benign prior to treatment.
Thyroiditis
Another form of hyperthyroidism is thyroiditis, a condition that occurs when your child’s thyroid gland becomes inflamed and causes excess thyroid hormone to leak into the bloodstream. While the source of the inflammation is often unknown, one rare type of thyroiditis, called subacute thyroiditis, can cause pain in your child’s thyroid gland. Most types of thyroiditis are painless and often resolve on their own, resulting in normal thyroid function.
Thyroid storm
There is a very rare, but severe and life-threatening form of hyperthyroidism called thyroid storm. Children with this condition have extremely high levels of thyroid hormone that can cause high fever, dehydration, diarrhea, rapid and irregular heart rate, shock and even death, if not treated. Patients with thyroid storm are cared for in the intensive care unit with intravenous fluids, steroids, non-radioactive iodine, beta-blockers and/or anti-thyroid medications.
Signs and symptoms of hyperthyroidism
Symptoms of hyperthyroidism may be mild or severe. In some cases, the severity of symptoms is not related to the level of thyroid hormone. Some children may have significant complaints with slightly elevated thyroid hormone levels, while others may report fewer symptoms with extremely elevated thyroid hormone levels.
Symptoms of hyperthyroidism may include:
- Enlarged thyroid (called a goiter)
- Increased heart rate or feeling the heart is "racing"
- Increased blood pressure
- Slight tremor
- Lighter and less frequent menstrual cycle for teens and young women
- Irritated and/or bulging eyes with redness or visible blood vessels on the white part of the eye, pain when moving the eyes, and inability to fully open the eye lid (Graves’ ophthalmopathy)
- Mood changes such as anxiety, irritability and nervousness
- Increased activity, fidgetiness, hyperactivity, restlessness
- Poor, restless sleep
- Fatigue
- Increased appetite — with or without weight loss
- Increased number of bowel movements per day
- Heat intolerance (always feeling warm)
- Decreased or poor school performance
- Difficulty concentrating; may be diagnosed with "late-onset" attention deficit disorder
- Feeling of a “lump” in the throat
Causes of hyperthyroidism
The vast majority of hyperthyroidism cases are caused by Graves’ disease (autoimmune hyperthyroidism).
Hyperthyroidism can also be caused by an autonomous nodule (a nodule functioning on its own), and by a non-immune inflammation, such as a viral or bacterial infection.
Hyperthyroidism and pregnancy
How does pregnancy affect hyperthyroidism?
It does not appear that pregnancy worsens hyperthyroidism or complicates treatment in women with this condition.
How does hyperthyroidism affect pregnancy?
Hyperthyroidism can have many effects on you and your baby. Some studies have shown an increase in pregnancy-induced hypertension (high blood pressure of pregnancy) in women with the disorder.
The stimulatory antibody, thyroid-stimulated immunoglobulin (TSI), that causes maternal hyperthyroidism can cross the placenta and affect the baby, leading to preterm birth (before 37 weeks of pregnancy), low birth weight, and neonatal Graves’ disease. While neonatal Graves’ disease is rare — affecting about 1 percent of babies born to mothers with active Graves’ disease or a history of the disease — if it is not diagnosed and treated promptly, the baby’s health can be at serious risk.
It is always best to plan for pregnancy and to consult with your physician to ensure your thyroid status and treatment are optimized prior to becoming pregnant and monitored throughout your pregnancy. However, if this does not happen and you find out you are pregnant, you should contact your physician immediately to arrange for increased testing of your thyroid functions and a potential change in your medication.
Management of hyperthyroidism during pregnancy
Treatment for hyperthyroidism is very specific to each patient. The goal of treatment is to maintain normal levels of thyroid hormone. Treatment may include:
- Frequent monitoring of thyroid levels throughout pregnancy
- Use of anti-thyroid drugs that help lower the level of thyroid hormones in the blood (certain drugs may affect the fetus and cause birth defects and should not be used)
- Surgery to remove all or part of the thyroid (if you have an overactive nodule)
Though radioactive iodine is an effective treatment for hyperthyroidism, it is not given to pregnant women to avoid harming the baby.
Women with hyperthyroidism can increase their chances for a healthy pregnancy by getting early prenatal care and working with their healthcare providers in the management of their disease.
For more information about Tyroid Disorders and Pregnancy, click here.
Testing and diagnosis
Diagnostic evaluation for hyperthyroidism begins with a thorough medical history and physical examination of your child. At Children’s Hospital of Philadelphia (CHOP), clinical experts use a variety of diagnostic tests to diagnose hyperthyroidism, including:
- Thyroid function screening, a blood test that measures thyroid hormone levels. Hyperthyroidism is diagnosed when the thyroid-stimulating hormone (TSH) level is below normal and the triiodothyronine (T3) and thyroxine (T4) levels are above normal. In "early" Graves’ disease, the T3 may be elevated before the T4. The presence of thyroid receptor antibodies (TRAb or TSH-receptor antibodies and/or TSI) help to confirm the diagnosis.
- Thyroid ultrasound, which uses ultrasonic waves to image your child’s thyroid and lymph nodes. An ultrasound does not expose your child to radiation. Classic findings of Graves’ disease include an enlarged thyroid gland with increased blood flow throughout the gland. Thyroid ultrasound is also the best test to screen for and identify thyroid nodules.
- Nuclear medicine uptake and scan, which helps determine how well your child’s thyroid tissue absorbs iodine, a key ingredient in making thyroid hormone. For the test, your child is given a very small amount of radioactive iodine — usually I-123 — then we measure how much iodine is absorbed (uptake) and the pattern of distribution of the radioiodine in the thyroid tissue (scan). Classic findings of Graves’ disease include increased absorption of the radioiodine (greater than 30 percent of thyroid hormone production at 24 hours) that is uniformly distributed throughout the thyroid tissue.
- Fine-needle aspiration, which uses a thin, hollow needle to take a small sample of thyroid cells. This test is usually only done when thyroid nodules are found during a thyroid ultrasound and is the best test to determine if the thyroid nodule is benign (non-cancerous) or malignant (cancerous).
Treatment of hyperthyroidism
At The CHOP, experts at the Pediatric Thyroid Center take a team approach to treatment for children with hyperthyroidism. Our board-certified endocrinologists, pediatric surgeons, nuclear medicine physician, and nurses collaborate to provide your child with individualized care and the best possible outcome.
Our Center is led by Andrew J. Bauer, MD, FAAP, a world-renowned endocrinologist and researcher, who is often sought for second opinions on difficult-to-diagnose thyroid disorders.
Depending on the cause of your child’s hyperthyroidism, treatment may include:
- Anti-thyroid medication
- Radioactive iodine ablation
- Total thyroidectomy (surgical removal of the thyroid) or lobectomy (removal of half of the thyroid gland)
Anti-thyroid medication
Most children and adolescents with hyperthyroidism will be started on anti-thyroid medication (Methimazole/Tapazole/MMI) at the time of diagnosis. For patients with severe symptoms, including elevated heart rate, palpitations and anxiousness, a medicine called a "beta-blocker" will be added to help decrease symptoms while the anti-thyroid medications take effect.
Up to 50 percent of patients treated with medications may eventually achieve remission, defined as resolution of hyperthyroidism for at least 18 months after stopping medication. Unfortunately, 30-40 percent of these patients — who appear to have their hyperthyroidism resolve — will experience a relapse.
Hyperthyroidism is harder to control in patients who are very young and have very high thyroid hormone levels at the time of their diagnosis. It is less likely for these patients to achieve remission of their disease, and more definitive treatments will be sought with the help of experts in the Pediatric Thyroid Center.
Children with hyperthyroidism who may need additional treatment include:
- Those who do not tolerate the anti-thyroid medication
- Those with disease that is difficult to control with the usual medical therapy
- Those who have not achieved remission despite prolonged medical therapy
Radioactive iodine ablation
Radioactive iodine (RAI) ablation is one of two options to permanently treat hyperthyroidism. Known as “definitive therapy,” RAI ablation medically destroys your child’s thyroid gland.
The benefits of RAI ablation include:
- It is an oral medication.
- It avoids surgery, so there is no risk of anesthesia and no scar for your child.
RAI ablation is not appropriate for all patients. Risks and concerns include:
- It takes longer for hyperthyroidism to resolve — usually two to three months.
- It is usually not offered to patients younger than 5 to 10 years of age.
- It may worsen eye disease associated with Graves’ disease.
- It is not as effective for large thyroid glands, which may need more than one dose of the medication.
- It is generally not recommended for children with both Graves’ disease and thyroid nodules.
- It is usually not used to treat hyperfunctioning thyroid nodules in children.
Thyroidectomy or lobectomy
Thyroidectomy is the second way to permanently treat hyperthyroidism. Lobectomy — or removal of half of the thyroid — is used to treat patients with a since autonomous nodule. Total thyroidectomy — removal of the entire thyroid gland — is used to treat patients with Graves' disease. Known as “definitive therapy,” thyroidectomy surgically removes all of your child’s thyroid gland. Lobectomy removes part of your child’s thyroid gland and is more often used to treat thyroid nodules.
The benefits of thyroidectomy and lobectomy include:
- Both offer quick resolution of hyperthyroidism. With thyroidectomy, there is no risk of needing a second procedure.
- There is no risk of eye disease related to Graves’ disease worsening.
- Thyroidectomy is the preferred treatment for children who have both Graves’ disease and thyroid nodules.
Thyroidectomy and lobectomy also have risks and concerns including:
- Your child will have a scar.
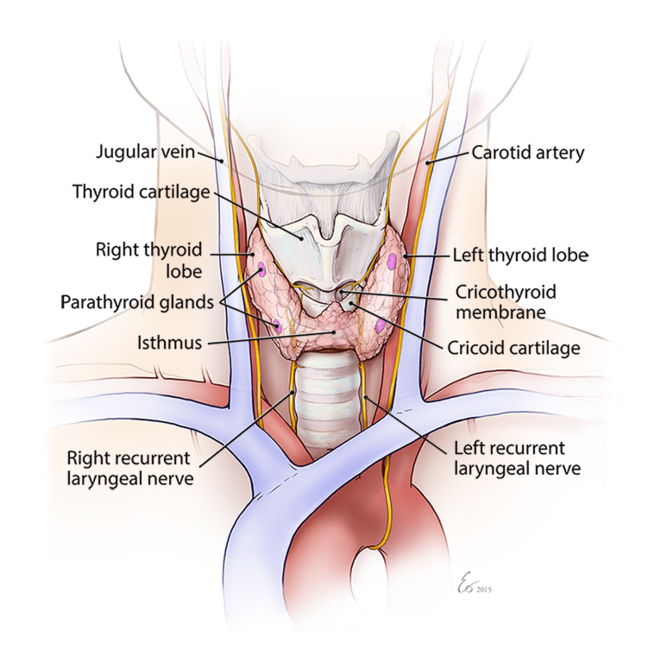
- There is a risk of surgical complications including hypoparathyroidism (damage to the parathyroid glands that control calcium) and recurrent laryngeal nerve damage (nerves that control the voice and help protect the airway so food, liquid or other items do not enter the lungs).
- It should be performed by high-volume surgical program (more than 30 thyroid surgeries per year) in a pediatric hospital setting, like the Pediatric Thyroid Center at CHOP, which has expert surgeons who can reduce the risk of complications.
To reduce the risk of surgical complications, thyroid surgery should be performed by an experienced surgeon who performs more than 30 thyroid surgeries a year and works in a pediatric hospital setting like the Pediatric Thyroid Center at CHOP.
Follow-up care for hyperthyroidism
Follow-up care for your child with hyperthyroidism will depend on the type of disorder your child has and the treatment your child received.
If your child is on anti-thyroid medication, she will need ongoing follow-up care to ensure her medication dosage is appropriate as she grows.
If your child received definitive therapy of RAI ablation or thyroidectomy, she will need to take thyroid hormone replacement for the rest of her life. If your child received a lobectomy, she may need to take thyroid hormone replacement. Thyroid hormone replacement is a once-a-day medication that requires less frequent dose adjustments and subsequently less frequent laboratory tests and doctor visits when compared to the treatment of Graves’ disease.
Follow-up care and ongoing support and services are available at our Main Campus and throughout our CHOP Care Network. Our team is committed to partnering with you to provide the most current, comprehensive and specialized care possible for your child.
Outcomes for hyperthyroidism
The majority of children with hyperthyroidism can be controlled within three to six months of initiating treatment. They can return to normal activities — including sports — once thyroid hormone levels are improving or have achieved normal levels, depending on the individual patient.
Up to 30 percent of patients who are treated with medication will not receive remission within 5 years of treatment. For these patients, definitive treatment (radioactive iodine ablation or surgery) may be needed.
There is a small group of patients who, despite having normal lab values after treatment for hyperthyroidism, still have symptoms. Dr. Bauer and a team of clinicians at CHOP are actively involved in thyroid disease research to learn more.
Resources to help
Hyperthyroidism Resources
Pediatric Thyroid Center Resources
We have created resources, including videos, to help you find answers to your questions and feel confident with the care you are providing your child.
Reviewed by Andrew J. Bauer, MD
