What is voiding dysfunction?
Voiding dysfunction is a general term that refers to abnormalities in the way your child’s bladder holds and releases urine. It can present in a variety of ways, including urinary frequency, urinary incontinence and urinary tract infections (UTI).
If your child is having trouble with bladder control or wetting accidents, rest assured they are not alone. About 20% of children over age five experience some form of bladder or urinary tract dysfunction. We understand how frustrating these problems can be for your child and family and we’re here to help.
The Dysfunctional Outpatient Voiding Education (DOVE) Center at Children’s Hospital of Philadelphia (CHOP) is among the largest, most comprehensive clinics in the United States devoted to pediatric bladder and urinary tract dysfunction. Our team of urologists, nurses, nurse practitioners and psychologists work together to sort out what is causing these problems and develop a treatment plan tailored to your child’s needs.
Causes of voiding dysfunction
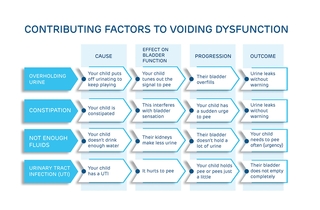
Sometimes behavior patterns that a child has developed over time can contribute to voiding dysfunction. For example, children who habitually put off urinating because they don’t want to stop playing to go to the bathroom may leak urine without warning. Children who don’t drink enough water may suffer from an urgent need to go because of their small bladder capacity.
Physical factors like constipation and urinary tract infections can also lead to voiding dysfunction.
Types of voiding dysfunction
Urinary urgency – When your child has uncontrolled bladder contractions that make them feel like they need to go to the bathroom “right now!”
Urinary frequency – When your child needs to go to the bathroom more than normal, given their age and health.
Urge incontinence – When your child leaks urine, makes frequent and urgent trips to the bathroom and attempts to hold the urine by doing things like crossing their legs, squatting and dancing to prevent leakage.
Giggle incontinence – Your child with giggle incontinence will wet ONLY when laughing. Once they start urinating, they are unable to stop the flow of urine and usually soak their clothes.
Stress incontinence – When urine leaks involuntarily during activities that increase abdominal pressure, like coughing, sneezing or exercising.
Dysfunctional voiding – When your child tightens their pelvic floor muscles as their bladder empties and cuts off the urine stream before completely emptying. A large amount of urine left in their bladder may leak after voiding.
Incomplete bladder emptying – When your child does not fully empty their bladder when they go to the bathroom, leaving residual urine behind.
Underactive bladder – When your child postpones voiding, has little urge to do so and only empties a few times a day.
Signs and symptoms of voiding dysfunction
The following signs and symptoms may signal that your child is experiencing voiding dysfunction:
- They have wetting accidents during the day when they are awake (daytime incontinence)
- They experience a frequent and urgent need to urinate (urinary frequency and urgency)
- They are bedwetting beyond the age when most children achieve nighttime dryness (nocturnal enuresis)
- They have pain or discomfort with urination (dysuria)
- They have difficulty starting their urine stream or keeping it going (hesitancy and straining)
When to seek care for voiding dysfunction
You should seek care for your child for voiding dysfunction if:
- They have persistent symptoms and continue to struggle with voiding issues beyond the typical age of bladder control
- They have pain or discomfort associated with urination
- You notice changes in your child’s behaviors related to their toileting habits
- Your child has accompanying symptoms including fever, abdominal pain or constipation
- Symptoms are impacting your child’s self-esteem
Testing and diagnosis for voiding dysfunction
The first step in correctly diagnosing your child’s type of voiding dysfunction is to review your child’s history and voiding diary. A voiding diary helps us understand your child’s urination habits over several days. Your child may undergo additional tests including:
- Uroflowmetry - This is a simple, non-invasive test used to measure the flow of your child’s urine. For this test, your child will pee on a special toilet that measures the speed and amount of urine they pass. This will tell us how well the bladder is working and can help detect problems with urination like difficulty emptying the bladder or a slow or weak urine stream.
- Postvoid bladder scan - An ultrasound of your child’s bladder done in our office after they’ve urinated to see if there is any urine left in their bladder.
- Abdominal X-ray - This can help us tell if your child is constipated.
- Ultrasound - This is often done if your child has had frequent urinary tract infections or a urinary tract infection accompanied by a fever.
- Video urodynamic study (VUDS) - This is a detailed study to help us understand how the bladder works when other tests have not led us to a diagnosis. During the test, pictures and videos are taken of your child’s bladder as it fills and empties.
Treatment for voiding dysfunction
Based on the results of your child’s evaluation, our DOVE Center team will develop a treatment plan tailored to your child’s needs, which may include:
- Education around how the body works - We uncover the mystery of what may be leading to symptoms or accidents to help your child engage in finding the right solution to their problem.
- Changing voiding/stooling habits - We recommend that children start stool softeners to treat underlying constipation. We will also help your child develop a schedule that incorporates regular voiding and stooling throughout the day.
- Increasing fluid intake - We will explain to your child why drinking water is important and make recommendations as to how much water they should drink each day.
- Biofeedback training - Biofeedback will teach your child to relax their pelvic floor muscles and is effective at helping children learn to empty their bladders completely. It reduces urgency, wetting and recurrent urinary tract infections.
- Behavior modification – If needed, a CHOP psychologist may work with you and your child to provide additional strategies that help identify and overcome barriers to sticking with the recommended treatment.
- Medication - We use medications to treat frequent urinary tract infections, overactive bladder and nighttime wetting.
Long-term outlook for children with voiding dysfunction
Most children with voiding dysfunction achieve normal bladder control once they learn to manage underlying conditions like constipation or urinary tract infections, using treatments including behavior modification, timed voiding, pelvic floor retraining and if needed, medications. Success is higher when children and parents follow the therapies we recommend. While growth and nervous system development will help to resolve most forms of voiding dysfunction by the time your child reaches adolescence, some may experience persistent or recurrent symptoms into adulthood.
Tips for parents of children with voiding dysfunction
You can help your child with voiding dysfunction by:
- Encouraging communication – Urge your child to communicate openly with you about any discomfort or concerns they have related to toileting.
- Establishing a routine - Set regular bathroom breaks to encourage healthy voiding habits.
- Staying calm and being supportive - Avoid punishing your child for accidents and provide positive reinforcement for progress.
Resources to help
DOVE Center for Voiding and Bladder Function Resources
We have created resources to help you find answers to your questions and feel confident in the care you are providing your child.
Reviewed by Jason Van Batavia, MD, MSTR
Reviewed on 06/30/2025
