Pediatric Thyroid Surgery
About thyroid surgery for children
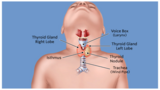
Thyroid surgery is the removal of all or part of the thyroid. The thyroid gland is a butterfly-shaped gland located in the front of your child’s neck, below the larynx (voice box). The small, two-inch gland consists of two lobes, one on each side of your child’s windpipe, connected by tissue called the isthmus. The thyroid plays an important role in regulating your child’s metabolism and calcium levels.
Pediatric thyroid surgery is a treatment option for children with thyroid cancer, thyroid nodules, or a thyroid disorder that doesn’t respond to other treatments.
Why your child may need thyroid surgery
Children with any of the following conditions may be recommended for thyroid surgery:
- Graves’ disease
- Thyroid nodules
- Benign (not cancerous)
- Malignant (cancerous)
- Indeterminate (uncertain if cancerous or not)
- Multiple endocrine neoplasia type 2 (MEN2), a hereditary cancer syndrome that is associated with certain types of thyroid cancers.
The type and extent of thyroid surgery will be determined by the disease and the results of diagnostic tests.
Total pediatric thyroidectomy
In a total thyroidectomy, a surgeon removes 99-100% of the thyroid gland. A total pediatric thyroidectomy is used to treat children with Graves’ disease, certain thyroid nodules, or if there is known thyroid cancer.
Pediatric thyroid lobectomy
In a pediatric thyroid lobectomy, a surgeon removes half of the thyroid gland, called a lobe. It is most often used to treat thyroid nodules, a firm lump in the thyroid gland.
A surgeon may perform a total thyroidectomy or a thyroid lobectomy when a child develops a thyroid nodule. Read more about thyroid nodule removal surgery.
What to expect during pediatric thyroid surgery
In pediatric thyroid surgery, a sideways incision is made in the base of the neck at the natural skin crease. The muscles in front of the thyroid gland are pushed aside to expose the thyroid gland.
Care is made to avoid damage to the delicate recurrent laryngeal nerves which run in the groove between the trachea and the esophagus. These nerves look like a strand of angel hair pasta. They control the vocal cords and help protect the airway so food, liquid or other items do not enter the lungs. At Children's Hospital of Philadelphia (CHOP), we use a special nerve monitoring device in the operating room to identify, confirm, and monitor motor nerve function to help reduce the risk of injury to the nerve during the procedure.
An important part of surgery is the successful location of the parathyroid glands, four tiny pea-shaped glands, each the size of a grain of rice, that are located in the neck behind the thyroid gland — two on top, two on the bottom. These glands share blood supply with the thyroid gland and produce a hormone that controls the amount of calcium in the blood. If they are damaged during surgery, the parathyroid gland can be temporarily or permanently shut down, resulting in lowered calcium levels.
Because of the precise nature of thyroid surgery, it is especially important to have an experienced pediatric surgeon perform the procedure. Our team of expert pediatric thyroid surgeons have extensive experience performing thyroid surgery in children. We also use a state-of-the-art handheld infrared light-emitting device that can accurately identify the tiny parathyroid glands.
After surgery
After surgical removal of most or part of the thyroid, the wound is stitched closed in layers using absorbable sutures. The sutures are underneath the skin and do not need to be removed. They will dissolve on their own over time. The top of the incision is covered with a thin white strip that is removed at home approximately one week after the surgery. The surgical scar is usually three to four centimeters in length and located in a skin fold to make it less noticeable.
The length of stay in the hospital will depend on if your child only had a thyroid lobe removed or the total thyroid gland removed. After thyroid lobectomy, serum calcium levels are not needed.
If your child had a total thyroidectomy, they will come back from the operating room with an IV that will allow us to check the calcium levels in the blood every six hours. When we are confident that calcium levels have normalized, your child will be ready for discharge to home. The typical hospital stay following total thyroid removal is one to two days.
Surgical pain usually goes away within the first few days and can typically be controlled with over-the-counter pain medication such as acetaminophen or ibuprofen. Most children return to school within days after surgery and resume full activity within one to two weeks. Thyroid wounds typically heal very well. Initially, the scar will be raised, firm, and darker in color. Over the course of several months, the scar will feel softer, look flatter, and have a lighter color. It is important to use sunscreen over the incision while exposed to the sun.
Why choose CHOP for pediatric thyroid surgery
There are clear differences in how a child or adolescent is treated when care is provided in a pediatric setting compared to an adult setting. Children’s Hospital of Philadelphia’s Pediatric Thyroid Center is one of the few centers in the nation dedicated to the unique medical needs of children and adolescents with thyroid disease. Our center provides the ideal combination of experience and resources, so we can provide individualized care for your child.
Our Thyroid Center houses a multidisciplinary team that specializes in caring for children with thyroid problems. Our pediatric endocrinologists are internationally recognized leaders in pediatric thyroid disease. For children who require surgery, finding a pediatric-trained surgeon is critical to achieving the best possible outcomes while reducing the potential risks of surgical complications, specifically, damage to the parathyroid glands and the recurrent laryngeal nerves.
The successful surgical outcomes of our patients also depend on several other team members. CHOP’s Department of Anesthesiology and Critical Care Medicine is a leader in pediatric anesthesiology and managing pain in children. If your child needs anesthesia, you can trust the experts in CHOP’s Division of General Anesthesiology to keep your child comfortable and safe before, during and after thyroid surgery. At Children’s Hospital of Philadelphia, we know children are not just small adults — and that children and infants have different needs than adults when it comes to anesthesia.
Our specially trained child life specialists are always available to be at your child’s side before surgery and after surgery. These important members of our team will do whatever they can to reduce the worry that is a normal part of undergoing thyroid surgery, and equip your child with helpful coping tools.
CHOP’s Division of Anatomic Pathology offers state-of-the-art consultative services and clinical diagnostic testing that has been proven to positively impact diagnostic outcomes for patients. Our pathology lab is staffed by highly experienced, board certified pathologists specializing in all aspects of pediatric pathology. This group works closely with other members of your child’s medical team to determine which tests will be most appropriate to confirm your child’s diagnosis and guide treatment.
An experienced surgical team will complete at least 30 thyroid surgeries per year. The surgeons at the Pediatric Thyroid Center at CHOP perform more than 80 thyroid surgeries a year. A recent article featured in the Journal of Pediatric Surgery illustrated our extraordinarily low complication rate after thyroidectomy – recurrent laryngeal nerve injury (0.4%) and permanent surgical hypoparathyroidism (0.6%). More than 700 thyroidectomies for thyroid nodules, thyroid cancer, and Graves’ disease have been performed by Drs. Adzick and Kazahaya since the Thyroid Center was established in 2009. We care for local, regional, national and international patients.


