Craniosynostosis Surgery
Surgical management for craniosynostosis is based on the suture(s) involved, the age of the child, and the individual needs for each patient.
The most commonly recommended options for treatment are the following:
Strip craniectomy
The common treatment approach at Children’s Hospital of Philadelphia (CHOP) includes a formal cranial vault expansion and reshaping procedure, but a strip craniectomy can be used as a preliminary procedure to reduce pressure in very young children (typically less than 6 months of age) with multiple sutures involved.
A strip craniectomy is typically performed in conjunction with a pediatric neurosurgeon. The procedure generally takes approximately two to three hours. After surgery, your child will stay at the hospital for recovery and follow-up care. Most children stay for an average of three to five days.
Additional surgeries including vault expansion and reshaping procedures will be scheduled according to your child’s recovery and response to this preliminary procedure.
Sagittal springs
Also known as cranial spring surgery.
The use of sagittal springs with strip craniectomy may be recommended for sagittal synostosis if the child is younger than 5 months at the time of initial surgery. The surgery involves a strip craniectomy and placement of two to three stainless steel springs to help increase the amount of room for the brain to grow, improve the skull shape, and reduce the risk of the sagittal suture closing again. Springs are an effective “minimally invasive” surgery that can be done through small incisions in the scalp, limit blood loss such that only a minority of patients require blood transfusion, and usually only results in a one-day hospital stay. There is an additional surgery approximately three months later to remove the springs.

Cranial molding helmet therapy may be used before surgery to limit the head shape progression associated with sagittal synostosis. Helmet therapy may also be used after spring removal to further redirect the skull growth to a more typical pattern.
Procedure demonstration of sagittal spring placement
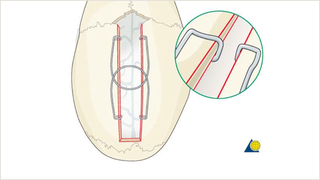
Demonstration of the bony cuts of the craniectomy and placement of sagittal springs. This procedure is used for correction of sagittal suture synostosis in early infancy.
Fronto-orbital advancement /reshaping
Fronto-orbital advancement may be used in the correction of metopic, coronal, or multi-suture craniosynostosis. It involves exposure of the upper eye socket and forehead through an ear-to-ear incision. The forehead bone is then removed with the assistance of the neurosurgeon. The misshapen upper eye socket is then cut free, reshaped, and replaced in a new position, held in place with resorbable plates and screws. The forehead is then reshaped and affixed to the upper eye socket.
This procedure offers eye protection by expanding the anterior skull to create room for brain growth, as well as reshapes the upper eye socket and forehead. For children with eye exposure, or ocular issues, the fronto-orbital advancement is a first-stage procedure. It is otherwise delayed as long as possible after posterior vault reconstruction and may be performed at an older age depending on other surgical procedures. A fronto-orbital advancement may be avoided for some diagnoses and instead managed with a monobloc with halo distraction at an older age.
A fronto-orbital advancement surgery takes approximately four to five hours, followed by a hospital stay of four to five days for monitoring and recovery. A surgical drain will be removed prior to discharge from the hospital. Additional surgeries may be needed as the child grows and further develops.


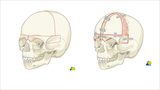
Procedure demonstration of fronto-orbital advancements

Demonstration of the bony cuts of a bilateral frontal orbital advancement are shown in red (left). On the right is a demonstration of the fixation of the reshaped frontal bones, held in place with resorbable plates and screws. Cranial bone graft cells are placed in the bony gap to help remodel this gap. This procedure is used most often for coronal synostosis and when the forehead is of a typical shape. From AO Surgery Reference (www.surgeryreference.aofoundation.org). Copyright by AO Foundation, Switzerland. Reprinted with permission.
Demonstration of the bony cuts of a bilateral frontal orbital advancement and broadening are shown
in red (left). On the right is a demonstration of the fixation of the reshaped frontal bones by resorbable screws and plates. A slurry of cranial bone cells is placed in the large bony gap to help remodel the bony gap. Used for correction of metopic synostosis, this procedure requires a reshaping of the forehead shape and therefore the extra need for fixation at the center of the forehead. From AO Surgery Reference (www.surgeryreference.aofoundation.org). Copyright by AO Foundation, Switzerland. Reprinted with permission.
Demonstration of the bony cuts of a bilateral frontal orbital advancement and broadening are shown in red (left). On the right is a demonstration of the fixation of the reshaped frontal bones, held in place with resorbable plates and screws. Cranial bone graft cells are placed in the bony gap to help remodel this gap. Used for correction of metopic synostosis, this procedure requires a reshaping of the forehead shape and therefore extra need for fixation at the center of the forehead. From AO Surgery Reference (www.surgeryreference.aofoundation.org). Copyright by AO Foundation, Switzerland. Reprinted with permission.
Demonstration of the bony cuts of a unilateral frontal orbital advancement (left-sided in this example)
are shown in red (left). On the right is a demonstration of the fixation of the reshaped frontal bones, held in place with resorbable plates and screws. Cranial bone graft cells are placed in the bony gap to help remodel this gap. Though not used at CHOP, this procedure may be used for unilateral coronal synostosis and when the forehead deformation is not severe, thus not needing bilateral reshaping. From AO Surgery Reference (www.surgeryreference.aofoundation.org). Copyright by AO Foundation, Switzerland. Reprinted with permission.
Cranial vault remodeling and reconstruction
Cranial vault remodeling, commonly called cranial vault reconstruction, involves the reshaping of cranial bones in a single stage surgery. This surgery is often used when more than one cranial suture closes prematurely. It involves a coronal (ear to ear) incision, followed by removal of the cranial bone by neurosurgery in the area that has been growth restricted. This procedure can be done regionally in the skull (for example, posterior skull remodeling, middle vault expansion, or anterior vault remodeling) or can be done to the total vault (whole skull).
After the bone is removed, the bone is reshaped and expanded. The reshaped skull is bolstered with a cranial bone graft and secured in place with resorbable plates or sutures to provide more room for brain growth and improvement in head shape. The surgery takes approximately four to five hours, followed by a hospital stay of four to five days for postoperative monitoring and recovery. After surgery, the child does not require cranial molding helmet therapy and can participate in sports without restriction when older.

Procedure demonstration of cranial vault reshaping and remodeling

Demonstration of the bony cuts of a posterior vault remodeling are shown in red (left). On the right is a demonstration of the fixation of the reshaped posterior vault bones, held in place with resorbable plates, screws, and sutures. In this example, treatment done for premature closure of the lambdoid suture.

Demonstration of the bony cuts of a posterior vault reshaping are shown in red (left). On the right is a demonstration of the fixation of the reshaped posterior vault bones, held in place with resorbable plates, screws, and sutures. In this example, treatment done for premature closure of the sagittal suture. Bilateral fronto-orbital advancement/reshaping may be required in a separate surgery if the anterior skull (front) is affected.
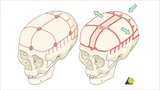
Demonstration of the bony cuts of a total cranial vault reshaping are shown in red (left). On the right is a demonstration of the direction of cranial vault expansion and shortening. In this example, treatment done for sagittal synostosis, but variation of this technique may be applied to various other forms of synostosis.
Posterior vault distraction osteogenesis
Posterior cranial vault distraction is a surgical procedure that expands the back of the skull by gradually stretching the bone and skin to expand the intracranial space and create new bone. CHOP has been a leader in instituting this procedure that has helped countless children.
Posterior cranial vault distraction is a less invasive surgery as compared to a formal open vault expansion and allows for significant expansion of the bone and soft tissue. The operation takes approximately two to three hours, with a hospital stay of three to five days. Starting three to five days after the procedure, your child’s surgeon will begin turning the distractors. This process will continue one to two times daily over the next two to three weeks, resulting in gradual expansion of the bone and soft tissue.
Caregivers continue turning the devices at home during the active distraction period, typically returning to the office weekly for skull X-rays and clinical examination. The distractors are then left in place for a period of consolidation to allow for solidification (hardening) of the new bone that was created.
Cranial distractors are removed in a second surgery approximately three months after the initial procedure.

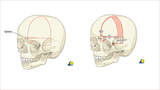
Procedure demonstration of posterior vault distraction
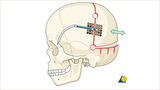
Demonstration of the bony cuts are shown in red and placement of posterior vault distractors (left). The green arrow represents the advancement that occurs with this procedure. This surgery is often used for correction of syndromic craniosynostosis given its ability to improve the shape and provide greater volume of expansion.
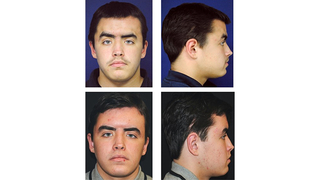
Final facial contouring
When your child is skeletally mature or done growing and all major osteotomies (bone cuts) are complete, final facial contouring may be needed to enhance the visual appearance and correct any remaining irregularities of the facial skeleton. Final contouring procedures including smoothing irregularities, reduction of contour abnormalities, adding bone grafts or bone substitutes, and re-suspending soft tissues.