Fetal surgery for spina bifida (myelomeningocele, MMC)
What is fetal surgery for spina bifida/myelomeningocele (MMC)?
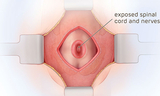
Fetal surgery for myelomeningocele (MMC) is a delicate surgical procedure done before a baby is born. MMC is the most common and severe form of spina bifida. In MMC, the fetus's spine doesn't fully form during pregnancy. As a result, part of the spinal cord and surrounding nerves stick out through an opening in the fetus's back. This exposes the spinal cord and nerves to amniotic fluid, which can cause damage.
In open fetal surgery for MMC, fetal surgeons open the uterus and close the opening in the baby's back while they are still in the womb. This protects the spinal cord from further damage from the amniotic fluid.
Fetal surgery for spina bifida is not a cure. However, studies of open fetal surgery show that fixing the hole in the spine before birth can offer better results than the traditional approach of fixing the hole after birth. Open fetal surgery for spina bifida greatly reduces fluid buildup in the brain and improves the chances that a child will be able to walk independently.
This video helps explain open fetal surgery for MMC. In it, our team members at Children's Hospital of Philadelphia (CHOP) talk about the treatment options for spina bifida. They list the benefits of having spina bifida surgery before birth. They explain why having the most experienced specialists perform this complex procedure is so important. And they detail all the support services we offer families along the way. The video also includes the perspective of families who have had the procedure.
Before fetal spina bifida surgery
Fetal surgery for spina bifida is a highly delicate, complex procedure. It is only available to certain patients. It takes a big commitment from mothers who choose to do it. It also takes deep surgical experience to perform.
For every fetal diagnosis of spina bifida, we carefully evaluate a range of factors related to the mother and fetus and then look at a variety of therapeutic options to repair the spina bifida defect. Options include open fetal surgery (which is what we cover in detail on this page); fetoscopic (minimally invasive) fetal surgery; and waiting until after the baby is born.
For specific guidelines around who is and is not eligible for open fetal spina bifida surgery, see our criteria for fetal surgery.
At CHOP, we do comprehensive testing and counseling to see if you meet the criteria. Your fetal therapy nurse coordinator will help guide you through each step.
You will have a physical exam and we will do a complete review of your medical history.
If you meet the criteria and are considering fetal surgery for MMC, we will make sure you have all the information you need to make your decision.
During a pre-surgery consultation, we will:
- Review the medications you will need to take before, during and after fetal surgery
- Go over the risks and potential complications of the surgical procedure (including preterm birth, uterine scarring, membrane separation, infection, bleeding, prematurity and fetal demise)
- Evaluate your mental state to make sure you are prepared for and have the coping mechanisms and family support needed to go through with the surgery
Choosing whether or not to go through with fetal surgery for MMC is a big decision. We created this list of questions to ask when considering your options for fetal surgery that can help you make the decision that is right for you and your baby.
If you are not a candidate for fetal surgery, we are still here for you and able to help. We will coordinate with your referring physician and follow the progression of your pregnancy. You will have the option of having surgery to repair the condition after birth here at CHOP.
Your fetal surgery care team
Fetal surgery for spina bifida takes a big team. Your care team will include fetal surgeons, neurosurgeons, maternal-fetal medicine specialists, fetal cardiologists, neonatologists, anesthesiologists, sonographers, advanced practice nurses, psychologists, social workers and fetal therapy coordinators. Each team member is focused on the best outcome for you and your baby. Your child also has access to every pediatric resource, no matter what additional care they may require.
About open fetal surgery for spina bifida
Open prenatal repair of myelomeningocele takes place between 23 weeks, and 25 weeks and 6 days gestation. Mothers must be willing to stay in Philadelphia with a support person for the surgery and the rest of the pregnancy. This allows us to monitor you closely.
In open prenatal repair, the mother receives general anesthesia. This sedates the mother, relaxes the uterus and anesthetizes the fetus. Fetal surgeons make an incision across the mother’s abdomen. A maternal-fetal medicine specialist uses ultrasound to locate the placenta and the fetus. The fetus's back is rotated into view. The uterus is then opened. A pediatric neurosurgeon removes the MMC sac if one is present. The neurosurgeon closes the layers of the back. The incisions in the uterus and the mother's abdomen are then closed.
During surgery, a fetal cardiologist uses echocardiography to monitor the fetus’s heart. This helps us keep both mother and baby safe.
After open fetal surgery, mothers usually stay in the hospital for three to five days. They must then stay on modified bed rest for three to four weeks. This reduces the risk of preterm labor. For the rest of the pregnancy, follow-up includes weekly appointments for ultrasound monitoring and routine prenatal care. If labor does not begin sooner, your baby will be delivered by planned cesarean section at 37 weeks. After delivery, your baby will be cared for in our Newborn/Infant Intensive Care Unit (N/IICU).
Watch the following video for more details about having open spina bifida surgery during pregnancy, including what to expect before, during and after the procedure.
After fetal surgery for spina bifida
Delivery of baby with MMC
Babies who have prenatal repair of MMC will be delivered in the Garbose Family Special Delivery Unit (SDU). This is the world’s first delivery unit within a pediatric hospital. It was created specifically for mothers carrying babies diagnosed with birth defects. Babies born in the Special Delivery Unit have access to the most advanced care immediately after delivery. You and your baby can also stay together in the same hospital for care after birth.
N/IICU stay
After your baby is born, they will stay in our Newborn/Infant Intensive Care Unit (N/IICU). They will be closely monitored by a team of specialists who have experience caring for babies with spina bifida. This team includes neurosurgeons, urologists, orthopedic specialists, physical therapists and others from the Spina Bifida Program.
Follow-up care after fetal spina bifida surgery
Mothers who choose open fetal repair at our center are encouraged to return to Philadelphia for evaluation of their child yearly if possible. Our Spina Bifida Program was the first multidisciplinary program in the nation. A team of specialists works together to provide the best long-term follow-up care for children.
This provides peace of mind that your child's health will be carefully followed. It also adds to our knowledge base to benefit future generations of children with spina bifida.
If you live further away from CHOP, our team will also ensure you have appropriate follow-up care for your child at a Spina Bifida Clinic close to home.
Prenatal spina bifida repair research
Our center co-led the landmark Management of Myelomeningocele Study, or MOMS study, that proved the benefits of performing open spina bifida surgery in utero. Follow-up studies continue to support those findings. They also show that the benefits of fetal surgery continue into school-age years. This ongoing follow-up and research is part of our commitment to the families we treat to ensure the best possible outcomes for every child.

Why choose CHOP for fetal surgery for spina bifida
If the baby you're carrying needs fetal surgery for spina bifida, we are here for you. Our surgeons helped create the procedure and have the most experience in the world.