What is gastroschisis?
Gastroschisis is a relatively uncommon condition that occurs in approximately 1 in 5,000 live births. It is one of a group of birth defects known as abdominal wall defects, which occur very early in gestation and are characterized by an opening in the abdominal wall of the fetus.
Most cases of fetal gastroschisis involve the intestine and other abdominal organs herniating (protruding) through an opening (hole) in the abdominal wall and spilling out into the amniotic fluid around the fetus. This opening is usually found to the right of the belly button. As a consequence, the unprotected intestine becomes irritated, causing it to swell and shorten.
The longer the exposure to amniotic fluid, the more likely the intestine will become damaged. In addition, as the fetus continues to develop, the tight opening may squeeze the blood supply to the intestine or cause it to twist around itself. Either of these consequences can cause inflammation, intestinal blockage, loss or malfunction and lead to long-term feeding problems after the baby is born.
Watch this educational video series to hear parents, nurses and doctors talk about abdominal wall defects and the treatment options available to your child at Children's Hospital of Philadelphia (CHOP). En Español »
Gastroschisis diagnosis
The diagnosis of gastroschisis is suspected after routine blood tests show abnormally high alpha fetoprotein levels. Gastroschisis is diagnosed by routine ultrasound in the second trimester when free-floating intestine is seen.

For proper counseling and management, it is important to distinguish gastroschisis from other abdominal wall defects, such as omphalocele (a membrane-covered herniation of the abdominal organs into the base of the umbilical cord).
Expectant mothers referred to CHOP's Center for Fetal Diagnosis and Treatment will undergo a comprehensive, one-day evaluation that includes a high-definition level II ultrasound to confirm the gastroschisis diagnosis and assess the intestine free-floating in amniotic fluid.
After the ultrasound, your family will meet with a high-risk obstetrician, pediatric surgeon and nurse coordinator who review test results, confirm the diagnosis, discuss options and potential outcomes and answer questions. Our team develops a treatment plan tailored to the specific needs of you and your baby. You will also receive educational information about gastroschisis and tour the Garbose Family Special Delivery Unit (SDU) and Newborn/Infant Intensive Care Unit (N/IICU) in upcoming visits.
Causes of gastroschisis
While there is no specific known cause of gastroschisis, it does not appear to run in families and the recurrence risk is not higher in future pregnancies. Gastroschisis occurs more often in babies born to younger mothers and the incidence of gastroschisis is increasing worldwide.
Unlike other abdominal wall defects, such as omphalocele, gastroschisis is typically not associated with chromosomal abnormalities or other structural malformations with the exception of an intestinal blockage (atresia), which occurs in only about 10 percent of infants with gastroschisis.
Management and delivery of babies with gastroschisis
The remainder of your pregnancy will be closely monitored. Your baby's intestine may become damaged because of exposure to the amniotic fluid. It is difficult to predict which babies are at risk for intestinal complications prenatally.
Pregnancies diagnosed with gastroschisis are at risk for certain complications such as poor fetal growth, decreased amniotic fluid volume, preterm delivery and stillbirth. Our center routinely monitors mothers starting at 28 to 32 weeks gestation with twice-weekly biophysical profiles and Doppler ultrasounds, keeping a close watch for signs of fetal distress.
We will partner with your local team of obstetricians and maternal-fetal medicine specialists to develop an individualized management plan designed to provide the best possible outcomes for your baby.
Depending on the severity of your baby’s case, you and your family may need to relocate to Philadelphia for a prolonged period of time for monitoring. Our experienced fetal therapy coordinators and social workers will help you navigate logistics and overcome barriers to care.
Our team of maternal-fetal medicine doctors, obstetricians, advanced practice providers and midwives provide expert maternal care with access to additional support services for your family, such as a psychologist or child life specialist.
If surveillance indicates issues with your pregnancy, our team is prepared to mobilize and move forward quickly to ensure the best outcome for you and your baby.
On average, spontaneous labor occurs around 36 weeks with gastroschisis. Most women deliver vaginally, unless there is a medical condition that necessitates a cesarean delivery or if your baby is having difficulty before birth.
At CHOP, delivery of babies with gastroschisis takes place in the Garbose Family Special Delivery Unit (SDU), allowing for expert obstetric services for the mother and the highest level of immediate care for the newborn — all within the same pediatric hospital. The world’s first birth facility designed exclusively for pregnancies complicated by birth defects, the SDU is a vital part of our team’s ability to provide comprehensive care for your whole family.
After birth, your baby is immediately moved from the delivery room to an adjacent stabilization room, where our Infant Stabilization Team will further stabilize your baby after assessment of breathing status and placing an intravenous (IV) line for fluids and nutrition. A nasogastric (NG) tube (a tube that runs through the nose) is placed to decompress the intestine, which prevents reflux of gastric contents into the lungs. Throughout the process, careful positioning of the baby is critical to maintain adequate blood flow to the intestine.
Once your baby is stabilized, they will be transported to the nearby Newborn/Infant Intensive Care Unit (N/IICU).
N/IICU stay for babies with gastroschisis
On arrival to the N/IICU, your baby will be in a specialized surgical patient area, with 24-hour surgical team coverage. The team evaluates level of breathing assistance needed, monitors medications and nutrition which are given through an IV (intravenous catheter inserted into a vein), and coordinates your child’s care throughout the hospital stay.

Neonatal Surgical Team
The Neonatal Surgical Team cares for babies who need surgery or other complex care immediately or soon after birth.
Parents are an integral part of the team and play an important role in caring for their baby from the start. During the stay in the N/IICU, a specialized team of surgeons, nurses, speech therapists (for feeding therapy), lactation consultants, respiratory therapists and social workers are available as needed to help educate your family about what you can do during the hospital stay, as well as caring for your baby after discharge. The nursing staff will help you learn special feeding techniques and other specialized care that your child might need.
Gastroschisis treatment
Repair of gastroschisis involves returning the extra-abdominal contents back into the abdominal cavity, followed by abdominal wall closure. This can either be performed with an immediate primary gastroschisis repair or, more commonly, a repair done in a series of steps (staged repair), depending upon postnatal assessment of the condition of the exposed intestine.
Primary gastroschisis repair
At the time of delivery, the exposed abdominal contents are placed in a moistened “bag” for your child's transfer to the N/IICU. In a primary gastroschisis repair, your baby undergoes surgical repair immediately upon admission to the N/IICU. The intestine is returned to the abdominal cavity and the abdominal wall is closed during one procedure.
Staged gastroschisis repair
Prenatal exposure of the fetal intestines to the amniotic fluid can be associated with bowel dilation and inflammation, thus making primary repair unfeasible. If the amount of bowel outside the abdomen is especially large or dilated or if your baby’s condition is unstable, a staged (done in several steps) approach will be performed over an average of five to 10 days.
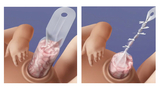
Upon admission to the N/IICU, a spring-loaded silastic (silicone plastic) pouch, commonly referred to as a “silo,” is placed around the herniated bowel. The bowel is then slowly and gently pushed back down into your child's abdomen over the course of a few days.
When all of the bowel has been reduced back into the abdomen, your surgeon will then discuss the options for closure of the abdominal wall. In babies with a small defect who required the silo for a short period of time, a “sutureless closure” can be performed with placement of a special dressing over the defect. This allows the abdominal wall to close spontaneously.
In babies with a larger defect and prolonged silo placement, your surgeon may recommend closure of the abdominal wall in the operating room, where the opening in the abdomen will be closed with stitches. It is not uncommon for babies to require breathing/ventilator assistance for a period of time after gastroschisis surgery.
Follow-up care for gastroschisis
After gastroschisis repair, it takes time for the intestine to recover and function normally. For this reason, first feedings are provided through an intravenous (IV) line. Once intestinal function returns, oral feedings or feedings via an NG tube are slowly started while IV feeds continue.
Pumping and freezing of breast milk is encouraged for feedings, because a mother's milk is particularly beneficial for infants with special medical needs. Oral feedings are slowly increased. This is a gradual process, and infants who have undergone gastroschisis repair might experience occasional setbacks, including the need to temporarily stop oral feeds to rest the intestine, or additional surgery.
When your baby can tolerate full feedings, whether oral, NG or a combination, with adequate weight gain, she is ready to go home. Prior to discharge, our nursing staff will teach you any special feeding techniques or other specialized care you may need to know to care for your child at home.
The length of stay in the hospital after gastroschisis repair varies, depending on a variety of factors:
- Whether your baby was born prematurely
- If there was any intestinal blockage (atresia)
- If there are feeding difficulties
After discharge from the hospital, your baby will be closely monitored by a pediatrician and will periodically return to CHOP for appointments with the pediatric surgeon.
Close attention will be paid to the condition of the intestine and your baby’s growth. While long-term prognosis can be very good, babies who sustained more severe injury to the intestine will need to be followed more closely and may need a prolonged course of intravenous nutrition either at home or within the hospital.

Tour our Fetal Center
The Wood Center for Fetal Diagnosis and Treatment has cared for many families and will help you through your journey, too.

What to expect
From the moment of referral through delivery and postnatal care, your family can expect a supportive experience when you come to us with a diagnosis of a birth defect.
Resources to help
Gastroschisis Resources
Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment Resources
Learning your baby has a birth defect is a life-changing experience. We want you to know that you are not alone. To help you find answers to your questions, we've created this list of educational health resources.
Reviewed by Deanna Ruble, BSN, RNC, Emily A. Partridge, MD, PhD, MHS


