What is ulcerative colitis?
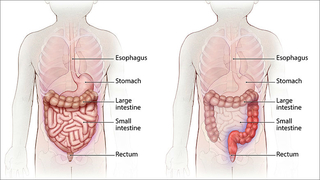
Ulcerative colitis belongs to a group of conditions known as inflammatory bowel disease (IBD). Ulcerative colitis is characterized by continuous segments of inflammation in the large intestine (colon) and the rectum. Only the innermost layer of the intestinal wall is affected.
In ulcerative colitis, the body’s immune system inappropriately targets the body’s healthy cells, thus signaling the body to attack them. This results in inflammation that can significantly affect a child’s quality of life.
Ulcerative colitis may affect as many as 907,000 Americans. It affects both males and females equally. Most are diagnosed in their mid-30s, but the disease can occur at any age and is becoming more common in children.
Causes of ulcerative colitis in children
Similar to other inflammatory diseases, the exact cause of ulcerative colitis is unknown, but research suggests that genetic, immunologic, and environmental factors are involved. Foreign substances (antigens) in the environment may directly cause inflammation, or they may “trigger” the body's defenses to produce inflammation that does not subside.
Once the immune system in a child with ulcerative colitis is “switched on," it may not know how to properly "switch off." As a result, the inflammation damages the tissues causing the symptoms of ulcerative colitis.
Signs and symptoms of ulcerative colitis in children
While the clinical signs of ulcerative colitis can vary from child to child, some symptoms may be more common than others, including bloody diarrhea. Other symptoms related to inflammation in the colon may include: abdominal pain, urgent or uncontrollable bowel movements, poor appetite, weight loss, and fatigue. Some children may experience less common symptoms, including skin rashes, joint pain, fatigue or fevers.
Ulcerative colitis is a chronic condition, meaning children may have periods of no symptoms (remission) alternating with periods of active symptoms (flare). Mild symptoms may present at first, while in other children, the onset of symptoms is more severe.
Testing and diagnosis of ulcerative colitis
Our team of gastroenterologists perform a thorough health history and physical examination and use a variety of tests to determine a diagnosis. Testing may include blood work, stool samples, imaging studies, and an endoscopy and colonoscopy with biopsies (a small piece of tissue sent to the lab to evaluate for inflammation). These tests help to identify laboratory abnormalities, including anemia or low blood protein levels, identify areas of the digestive tract with active inflammation, and determine if there is a contributing infection.
Imaging studies, such as magnetic resonance enterography (MRE) and video capsule endoscopy provide a detailed picture of the small intestine. These, along with an endoscopy and colonoscopy, offer a head to toe look at the inside of the body. Our child life specialists provide age-specific educational resources to assist in coping and psychosocial support with procedures.
The diagnosis may be difficult to confirm at first, which is why we use a variety of tests. In some cases, it may also be difficult to distinguish ulcerative colitis from Crohn’s disease, the other common type of inflammatory bowel disease.
Treatment for ulcerative colitis
The treatment for ulcerative colitis is complex and may be different for every child, but the main goals are the same: to relieve symptoms, prevent flares, and achieve mucosal healing (healing of the intestine) and remission. There is no “one size fits all” treatment for ulcerative colitis, and children respond to therapy differently. Using a combination of medication, nutritional therapy, and in more severe cases, surgery, we aim to promote each child’s quality of life without limiting his or her goals or dreams.
Primary treatment for ulcerative colitis includes medications. Those most often used in the treatment of ulcerative colitis are 5-aminosalicylates, corticosteroids, antibiotics, and medications that alter the immune system, called immunomodulators or biologics.
Medications to treat ulcerative colitis
When treating ulcerative colitis with medications, our goals are to suppress inflammation, heal tissue, and relieve symptoms. Commonly used medications include:
- 5-Aminosalicylic acid (5-ASA): Given orally or rectally, to decrease inflammation in mild or moderate cases
- Corticosteroids: Given topically, orally, or intravenously (IV) to quickly decrease inflammation in moderate to severe cases
- Antibiotics: Given orally or IV to reduce intestinal bacteria, suppress the immune system, and treat infection
- Immunomodulators: Given orally or by injection to weaken the activity of the immune system to decrease inflammation
- Biologic agents: Given by injection or through a vein to stop the inflammatory reaction in moderate to severe cases
Nutrition
Diet plays a big role in the treatment of ulcerative colitis. It is essential to maintain good nutrition because it helps the body to heal and grow. Weight loss is a common symptom of ulcerative colitis, and weight gain is a goal of treatment. Research supports the role of nutrition in treatment for ulcerative colitis. There is not one specific diet for ulcerative colitis. We have IBD dietitians who work closely with families in nutritional support.
Surgery to treat ulcerative colitis
Even with proper medication and diet, some children require surgery to attain the best possible quality of life. The decision to proceed with surgery is made in collaboration between the child and family, the gastroenterologist, and the surgeon specializing in IBD. Surgery is used to relieve severe, ongoing symptoms and to help children achieve growth and weight gain when medical management is no longer effective on its own. Unlike Crohn’s disease, in which surgery is a temporary solution, surgery can provide long-term relief with ulcerative colitis.
There are multiple surgical options for the treatment of ulcerative colitis. At the Center for Pediatric Inflammatory Bowel Disease, our team will work closely with your family to determine if surgery is necessary, and our expert surgeons who specialize in IBD-related procedures will provide additional information and work to optimize your child’s quality of life. Learn more about J-pouch Surgery and Bowel Resection Surgery.
Follow-up care for children with ulcerative colitis
Children treated for ulcerative colitis at CHOP receive long-term disease management through the Center for Pediatric Inflammatory Bowel Disease. A specialized team of pediatric IBD experts, including physicians, nurses, dietitians, psychologists, and social workers works together on the long-term management of your child's ulcerative colitis. Our team has an improved ability to schedule quicker appointments at The Buerger Center for Advanced Pediatric Care and our conveniently located CHOP Care Network centers with physicians who are renowned scientists and researchers pursuing new therapies and advancements in treatments. We provide ongoing monitoring of symptoms and treatment, a well-developed nutrition plan, multidisciplinary care, and support groups for the entire family. Our goal is to positively impact the physical and social health of your family and child.
Resources to help
Ulcerative Colitis in Children Resources
Center for Pediatric Inflammatory Bowel Disease Resources
We have collated resources to help you find answers to your questions about IBD and feel confident with the care you are providing for your child.
Reviewed by Andrew B. Grossman, MD, Judith R. Kelsen, MD

