
The many tiny bubbles percolating in a glass of champagne serve as a simplified illustration for microbubbles used as contrast agents in ultrasound. The major differences between the champagne and ultrasound contrast agent bubbles are the much smaller size and longer lasting properties of the ultrasound microbubbles. Their shells are made of lipid or protein, and they are filled with an inert gas. The microbubbles are smaller than red blood cells. In just 1 milliliter of suspension of a commonly used ultrasound contrast agent there are about 500 to 600 million microbubbles. These can be administered into the body via different routes and enhance the ultrasound reflection of the sound waves, resulting in an ultrasound image with high echogenicity, ie, contrast.
The use of ultrasound contrast agents in pediatric imaging began in Europe in the 1990s. However, the U.S. Food and Drug Administration (FDA) did not approve the use of an ultrasound contrast agent in children until 2016. The approvals were for intravenous administration for liver imaging and intravesical use for the diagnosis of vesicoureteral reflux. Since the FDA approval, the use of ultrasound contrast agents in the United States for the approved indications, as well as for additional off-label use, has grown at a rapid pace.
At the Department of Radiology at Children’s Hospital of Philadelphia, we have been using ultrasound contrast agents for more than 5 years. To consolidate the activities at CHOP targeting contrast enhanced ultrasound (CEUS), we established the Center for Pediatric Contrast Ultrasound (CPCU) that encompasses the Divisions of Body Imaging and Interventional Radiology in the Department of Radiology, as well as the Division of Emergency Medicine in the Department of Pediatrics. The CPCU has a trifold mission focused on pediatric CEUS: advance clinical applications, provide educational opportunities, and support research activities.
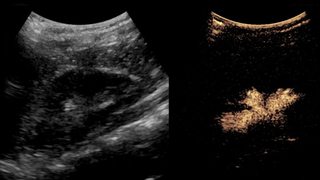
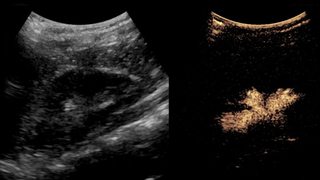
The most common intravenous application is to diagnose focal liver lesions (see Figure 4). After injection of the microbubbles, it is possible to see in real time the enhancement pattern of the focal lesion in the arterial, portal-venous, and delayed phases to determine what the lesion is. Blunt abdominal trauma is evaluated by depicting nonenhancing areas in all of the parenchymal organs and is a very sensitive, fast, and easy-to-do imaging modality (see Figure 5). Additional indications in the abdomen include mass lesions and inflammation in the spleen, pancreas, adrenals, kidneys (see Figure 6), bladder, uterus, and testes. Ultrasound contrast agents also are useful in the assessment of disease activity of the bowel in Crohn’s disease. Additional emerging applications include brain and hip scans for possible ischemia.
For intravesical administration of ultrasound contrast agent, contrast-enhanced voiding urosonography (ceVUS) is the most widespread contrast ultrasound exam in children. It is not only a more child-friendly study without radiation, but also is more sensitive in detecting vesicoureteral reflux compared to conventional methods. Further expansion of this method includes contrast enhanced genitosonography for evaluation of complex urogenital anomalies by filling different cavities with the contrast agent. The use of the microbubbles in pediatric interventional radiology includes targeted biopsy, depiction of line and tube positions, assessment of organ ischemia post intervention, and many others. Recently, we started using intralymphatic ultrasound contrast agent to direct needle placement in an inguinal lymph node for MR lymphangiography or evaluate the patency of the thoracic duct.
Monthly for the past 2 years, the CPCU has carried out 1-day, hands-on pediatric contrast ultrasound workshop for small groups. The workshop incorporates a detailed how-to part, in-vitro and phantom demonstrations of contrast ultrasound, and live patient exams. To date, more than 100 pediatric radiologists and sonographers from around the nation have been trained. This workshop has been instrumental in facilitating the establishment of CEUS for more than 40 centers in the United States.
The research on contrast ultrasound has significantly expanded. The basic science research has ventured into the evaluation of the fetal brain perfusion in a lamb model in the setting of research being done by the CHOP Center for Fetal Diagnosis and Treatment. We have prospective studies under FDA Investigational New Drug approval as well as many retrospective ones. In the past 2 years, the CPCU supported garnering research grants from 13 different sources amounting to more than $3 million. At the annual meeting of the Society for Pediatric Radiology this year, the top 2 research awards were for contrast US and both were awarded for work done at CHOP.
In a short period, tiny bubbles are indeed making significant impact on pediatric imaging not only at CHOP, but—under CHOP’s leadership—also at many institutions nationwide.


Contributors also included Aikaterini Ntoulia, MD, PhD
Featured in this article
Specialties & Programs
The many tiny bubbles percolating in a glass of champagne serve as a simplified illustration for microbubbles used as contrast agents in ultrasound. The major differences between the champagne and ultrasound contrast agent bubbles are the much smaller size and longer lasting properties of the ultrasound microbubbles. Their shells are made of lipid or protein, and they are filled with an inert gas. The microbubbles are smaller than red blood cells. In just 1 milliliter of suspension of a commonly used ultrasound contrast agent there are about 500 to 600 million microbubbles. These can be administered into the body via different routes and enhance the ultrasound reflection of the sound waves, resulting in an ultrasound image with high echogenicity, ie, contrast.
The use of ultrasound contrast agents in pediatric imaging began in Europe in the 1990s. However, the U.S. Food and Drug Administration (FDA) did not approve the use of an ultrasound contrast agent in children until 2016. The approvals were for intravenous administration for liver imaging and intravesical use for the diagnosis of vesicoureteral reflux. Since the FDA approval, the use of ultrasound contrast agents in the United States for the approved indications, as well as for additional off-label use, has grown at a rapid pace.
At the Department of Radiology at Children’s Hospital of Philadelphia, we have been using ultrasound contrast agents for more than 5 years. To consolidate the activities at CHOP targeting contrast enhanced ultrasound (CEUS), we established the Center for Pediatric Contrast Ultrasound (CPCU) that encompasses the Divisions of Body Imaging and Interventional Radiology in the Department of Radiology, as well as the Division of Emergency Medicine in the Department of Pediatrics. The CPCU has a trifold mission focused on pediatric CEUS: advance clinical applications, provide educational opportunities, and support research activities.
The most common intravenous application is to diagnose focal liver lesions (see Figure 4). After injection of the microbubbles, it is possible to see in real time the enhancement pattern of the focal lesion in the arterial, portal-venous, and delayed phases to determine what the lesion is. Blunt abdominal trauma is evaluated by depicting nonenhancing areas in all of the parenchymal organs and is a very sensitive, fast, and easy-to-do imaging modality (see Figure 5). Additional indications in the abdomen include mass lesions and inflammation in the spleen, pancreas, adrenals, kidneys (see Figure 6), bladder, uterus, and testes. Ultrasound contrast agents also are useful in the assessment of disease activity of the bowel in Crohn’s disease. Additional emerging applications include brain and hip scans for possible ischemia.
For intravesical administration of ultrasound contrast agent, contrast-enhanced voiding urosonography (ceVUS) is the most widespread contrast ultrasound exam in children. It is not only a more child-friendly study without radiation, but also is more sensitive in detecting vesicoureteral reflux compared to conventional methods. Further expansion of this method includes contrast enhanced genitosonography for evaluation of complex urogenital anomalies by filling different cavities with the contrast agent. The use of the microbubbles in pediatric interventional radiology includes targeted biopsy, depiction of line and tube positions, assessment of organ ischemia post intervention, and many others. Recently, we started using intralymphatic ultrasound contrast agent to direct needle placement in an inguinal lymph node for MR lymphangiography or evaluate the patency of the thoracic duct.
Monthly for the past 2 years, the CPCU has carried out 1-day, hands-on pediatric contrast ultrasound workshop for small groups. The workshop incorporates a detailed how-to part, in-vitro and phantom demonstrations of contrast ultrasound, and live patient exams. To date, more than 100 pediatric radiologists and sonographers from around the nation have been trained. This workshop has been instrumental in facilitating the establishment of CEUS for more than 40 centers in the United States.
The research on contrast ultrasound has significantly expanded. The basic science research has ventured into the evaluation of the fetal brain perfusion in a lamb model in the setting of research being done by the CHOP Center for Fetal Diagnosis and Treatment. We have prospective studies under FDA Investigational New Drug approval as well as many retrospective ones. In the past 2 years, the CPCU supported garnering research grants from 13 different sources amounting to more than $3 million. At the annual meeting of the Society for Pediatric Radiology this year, the top 2 research awards were for contrast US and both were awarded for work done at CHOP.
In a short period, tiny bubbles are indeed making significant impact on pediatric imaging not only at CHOP, but—under CHOP’s leadership—also at many institutions nationwide.


Contributors also included Aikaterini Ntoulia, MD, PhD
Contact us
Department of Radiology