Physical Activity Eases Foot Pain, But Makes Knee Pain Worse
Published on
Children's DoctorPublished on
Children's DoctorAn 11-year-old boy presented with 2 months of foot and knee pain. His foot pain was worse in the morning, accompanied by morning stiffness, and improved with physical activity. The knee pain was worse after activity. On examination the foot was warm and swollen. His knee was not swollen, but there was tenderness at the distal patella. Labs were unremarkable, including Lyme, rheumatoid factor, and ANA. He was prescribed naproxen and referred to Rheumatology.
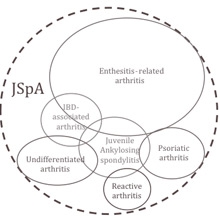 Figure 3: The overlapping symptoms of juvenile spondyloarthritis (JSpA).
Discussion: This patient had juvenile spondyloarthritis. Spondyloarthritis accounts for 15% to 20% of juvenile arthritis and encompasses a group of conditions characterized by arthritis with varying amounts of inflammation at tendon insertions into bone (enthesitis), sausage-like swelling of the digits (dactylitis), psoriasis, inflammatory bowel disease, back pain, and painful eye inflammation (acute uveitis) (See Figure 3). Unlike other types of juvenile arthritis, spondyloarthritis preferentially affects boys, and the peak age of onset is early adolescence. In comparison to other types of arthritis, children with spondyloarthritis are less likely to achieve and sustain remission.
Figure 3: The overlapping symptoms of juvenile spondyloarthritis (JSpA).
Discussion: This patient had juvenile spondyloarthritis. Spondyloarthritis accounts for 15% to 20% of juvenile arthritis and encompasses a group of conditions characterized by arthritis with varying amounts of inflammation at tendon insertions into bone (enthesitis), sausage-like swelling of the digits (dactylitis), psoriasis, inflammatory bowel disease, back pain, and painful eye inflammation (acute uveitis) (See Figure 3). Unlike other types of juvenile arthritis, spondyloarthritis preferentially affects boys, and the peak age of onset is early adolescence. In comparison to other types of arthritis, children with spondyloarthritis are less likely to achieve and sustain remission.
The arthritis of spondyloarthritis is usually oligoarticular (<5 joints), involves the lower extremities, and may include the spine or lower back. Hip and small joint arthritis of the midfoot (tarsitis) are highly suggestive of the diagnosis. One-third of these children develop arthritis of the lower back (sacroiliitis). In a child diagnosed with spondyloarthritis, elevated C-reactive protein and HLA-B27 positivity should prompt evaluation for sacroiliitis. Children with untreated sacroiliitis are at risk for progression to ankylosing spondylitis, which is characterized by fusion of the pelvic joints. HLA-B27 positivity increases the likelihood of developing sacroiliitis; however, many children who are HLA-B27+ never develop spondyloarthritis. The presence of back pain is not as helpful in signaling the onset of sacroiliitis in children as in adults with spondyloarthritis. Several studies, including one from our team at CHOP, have reported that up to 20% of children with imaging-confirmed sacroiliitis (X-ray or MRI) have never experienced back pain.
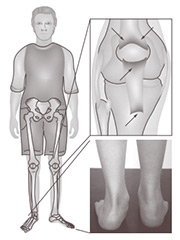 Enthesitis is a unique characteristic of spondyloarthritis (See Figure 4). The most commonly affected sites are at the distal patella (attachment of infrapatellar tendon), bottom of the heel (attachment of plantar fascia), and the back of the heel (attachment of Achilles tendon). Pain from enthesitis, unlike arthritis, is worse at the end of the day and after activity. Physical exam findings may include pain with palpation or swelling at the tendon insertion.
Enthesitis is a unique characteristic of spondyloarthritis (See Figure 4). The most commonly affected sites are at the distal patella (attachment of infrapatellar tendon), bottom of the heel (attachment of plantar fascia), and the back of the heel (attachment of Achilles tendon). Pain from enthesitis, unlike arthritis, is worse at the end of the day and after activity. Physical exam findings may include pain with palpation or swelling at the tendon insertion.
Figure 4: Children with spondyloarthritis frequently have enthesitis (arrows). Photo shows swelling at the site of the Achilles tendon insertion. Figure adapted from Tse SM, Laxer RM. New advances in juvenile spondyloarthritis. © 2012 by Nat Rev Rheumatol. 2012;8(5):269-279. Reprinted with permission.
There are also several extra-articular manifestations of spondyloarthritis of which primary care pediatricians should be aware. Uveitis occurs in one-quarter of children with spondyloarthritis and is characterized by acute-onset redness, pain, and photosensitivity. Approximately two-thirds of children with spondyloarthritis have intestinal inflammation. The prevalence of psoriasis in juvenile spondyloarthritis is uncertain but affects 10% to 25% of adults. Other spondyloarthritis-associated conditions include chronic recurrent multifocal osteomyelitis and psoriasis.
Goals of treatment are to reduce discomfort and inflammation and to prevent joint damage and dysfunction. Nonsteroidal antiinflammatory drugs (NSAIDs) such as naproxen and ibuprofen are effective for short-term relief of pain, particularly for enthesitis. NSAIDs are not sufficient therapy for the treatment of active arthritis. Studies in adults suggest continuous NSAID use reduces the radiographic appearance of spinal inflammatory lesions and may slow spinal radiographic progression, but this has not been evaluated in children. Corticosteroid injection into a joint(s) may provide rapid relief for disabling arthritis (ie, swollen wrist that prevents writing). For children who require repeat injections or with 5 or more affected joints, a disease-modifying drug such as methotrexate is recommended. For lower back or spinal arthritis, initiation of a tumor necrosis factor inhibitor such as etanercept, adalimumab, or infliximab is recommended. Drugs that target the IL-17 axis have shown promising results in adult studies and may have applicability in children in the near future.
Our patient was HLA-B27+ and had enthesitis of the infrapatellar and Achilles tendon insertions and tarsitis of the foot. He was started on methotrexate and naproxen. At the 12-week follow-up, his ankle, foot, and knee pain had resolved. Six months later he developed lower back pain and elevated C-reactive protein. MRI of the pelvis demonstrated periarticular bone marrow edema and sclerosis of the sacroiliac joints. Etanercept was added to methotrexate therapy. Repeat MRI 3 months later showed resolution of bone marrow edema. He has been asymptomatic for the past 2 years. Rheumatology will continue to follow him until transition to adult care since long-term remission off medication for spondyloarthritis is uncommon.
Gmuca S and Weiss PF. Juvenile Spondyloarthritis. Curr Opin Rheumatol. 2015;27(4):364-372
Tse SM and Laxer RM. New Advances in juvenile spondyloarthritis. Nat Rev Rheumatol. 2012. 8(5):269-279.
Weiss PR, Xiao R, Biko DM, Chauvin NA. Sacroiliitis at diagnosis of juvenile spondyloarthritis assessed by radiography, magnetic resonance imaging, and clinical examination. [Published online ahead of print July 20, 2015.] Arthritis Care Res (Hoboken).
To refer a patient to the Division of Rheumatology, call 215-590-2547. For information on the division’s services and clinicians, go to www.chop.edu/rheumatology.
Contributed by: Pamela F. Weiss, MD, MSCE
Categories: Rheumatology, Children's Doctor Winter 2016