What is thyroid cancer?
Thyroid cancer is abnormal cell growth in the thyroid, a butterfly-shaped gland in the front of the neck. The thyroid produces hormones that play an important role in helping to regulate the body’s growth and metabolism. In some cases, thyroid cancer can spread from the thyroid to other parts of the body.
Pediatric patients with thyroid cancer, no matter how far the cancer has spread, typically respond well to treatment. The goal of evaluation and treatment is to personalize care based on the behavior of the thyroid cancer in each specific patient and to reduce the risk of complications. Our goal is that all of our thyroid cancer patients will go on to lead productive and rewarding lives.
Types of thyroid cancer in children
Thyroid cancer in children is grouped into four types:
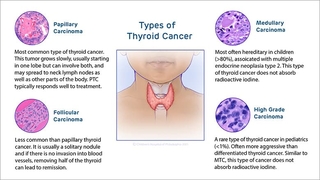
- Papillary thyroid cancer (PTC) is the most common type of thyroid cancer in children and adolescents, accounting for 90% to 95% of all diagnoses. Teenage girls are more likely to develop papillary thyroid cancer compared to boys or younger children of either sex. In papillary thyroid cancer, the tumor grows slowly, usually starting in one lobe but sometimes involves both lobes. PTC often spreads to lymph nodes in the neck and, less commonly, to other parts of the body, including the lungs. Papillary thyroid cancer typically responds well to treatment.
- Follicular thyroid cancer (FTC) is less common than papillary thyroid cancer. It is usually found as a solitary nodule in just one of the thyroid lobes. In contrast to PTC, when FTC spreads, it travels through blood vessels to other parts of the body, including the lungs and bones. When there is no evidence of invasion into blood vessels in the tumor, removing the affected lobe can lead to remission.
- Papillary and follicular thyroid cancers are classified as differentiated thyroid cancer (DTC) with both originating from the thyroid hormone-producing cells of the gland. In most patients, we do not identify a reason for the DTC developing, however, risk factors include exposure to radiation prior to 10-years of age as well as several familial predisposition tumor syndromes.
Family history of thyroid cancer
Once a family member is diagnosed with either papillary or follicular thyroid cancer, there appears to be a small—but significant—rick of other family members developing the same type of cancer. The risk may be isolated to the development of thyroid cancer or may be associated with an increased risk of developing other forms of cancer or thyroid-related medical conditions such as including PTEN hamartoma tumor syndrome, DICER1-related tumor predisposition syndrome and familial adenomatous polyposis.
- Medullary thyroid cancer (MTC) is most often hereditary when it occurs in children, associated with a tumor syndrome called multiple endocrine neoplasia type 2. It begins in cells that play a role in regulating calcium levels in the body. Medullary thyroid cancer can spread to lymph nodes and other parts of the body. Because the cells it begins in do not absorb iodine, medullary thyroid cancer is treated with surgery as well as oral chemotherapy if it spreads to distant sites. Children will be followed by CHOP’s Advanced Pediatric Thyroid Cancer Therapeutics Clinic.
- High-grade follicular-derived carcinoma is rare in children (less than 1% of all thyroid cancer diagnoses) and is more aggressive than differentiated thyroid cancer. It arises from papillary or follicular cancer and can spread to lymph nodes and other parts of the body. Similar to MTC, poorly differentiated thyroid carcinoma and differentiated high-grade thyroid carcinoma often to not respond to radioiodine therapy.
Signs and symptoms of thyroid cancer in children
Most children and adolescents with thyroid cancer do not have any obvious signs or symptoms. In most cases, a lump in the neck is noticed during a physical exam or through a radiology study for an unrelated issue and is determined to be a thyroid nodule.
When signs/symptoms are present, they may include:
- A visible lump in the neck
- The sensation of a lump in the neck when swallowing or lying down
- Hoarseness or another change in the voice
For certain inherited forms of medullary thyroid cancer, additional physical signs and features may be present.
Causes of thyroid cancer in children
For the majority of children, close to 90%, there is not an identifiable reason the cancer developed. For the 10% of children who have an identifiable cause, genetic factors have been associated with the development of some types of thyroid cancer in children, including most cases of medullary thyroid cancer and some cases of differentiated thyroid cancer, or the child had exposure to radiation for treating another type of cancer.
Risk factors can increase your child’s risk of developing thyroid cancer. These include:
- Exposure to ionizing radiation in the head and neck as part of previous treatment for another form of cancer. Patients less than 10 years of age at the time of exposure are at greatest risk.
- Familial tumor predisposition syndrome, including PTEN hamartoma tumor syndrome, DICER1-related tumor predisposition syndrome and familial adenomatous polyposis associated with differentiated thyroid cancer and multiple endocrine neoplasia type 2 associated with medullary thyroid cancer.
- Autoimmune thyroid disease, including Hashimoto’s thyroiditis (also known as chronic lymphocytic thyroiditis).
Testing and diagnosis of thyroid cancer
Diagnosis of thyroid cancer begins with a complete medical history and comprehensive physical examination that includes evaluation of the thyroid and the lymph nodes in the neck. Watch CHOP Endocrinologist Andrew J. Bauer, MD, perform a pediatric thyroid exam.
Diagnostic tests may include:
- Blood test to measure the thyroid-stimulating hormone (TSH) level to determine how well your child’s thyroid is working.
- Thyroid ultrasound to learn about the size, number, appearance and location of any thyroid nodules and abnormal lymph nodes.
- Fine needle aspiration (FNA) to collect cells from the thyroid, and possibly lymph nodes, to be examined under a microscope.
- A nuclear medicine uptake and scan will be ordered if your child’s TSH level is low or suppressed. This test determines if the thyroid nodule is absorbing an increased amount of iodine.
Treatment for thyroid cancer
Treatment for thyroid cancer may include:
- Surgery to remove one of the two thyroid lobes (called a lobectomy) or the entire thyroid (called a total thyroidectomy).
- Radioactive iodine treatment to destroy remaining thyroid cells after surgery. Radioactive iodine treatment is only recommended for patients with an intermediate or high likelihood of having persistent post-surgery thyroid cancer.
- Thyroid hormone replacement therapy to supply your child with necessary growth- and metabolism-regulating hormones after thyroid-removal surgery. You child may require thyroid hormone suppressive therapy to reduce the risk that any remaining cancer cells will grow.

What to expect
Learn about what to expect during and how to prepare for your child's appointment with the Pediatric Thyroid Center at CHOP.
Follow-up care for thyroid cancer
All children treated for thyroid cancer will need long-term follow-up care into adulthood. In the first few years after surgery, your child will require physical exams, laboratory tests and radiological imaging every three to six months.
Follow-up exams may become yearly if there is no evidence of persistent or recurrent cancer. Your child’s healthcare team will customize a follow-up plan based on your child’s condition and outcome.
Many children will achieve remission, that is, they will have no evidence of thyroid cancer. However, others may develop persistent or recurrent thyroid cancer, and the cancer may spread to other organs, most commonly the lungs.
Patients who develop persistent thyroid cancer that does not respond to typical treatments will be referred to the Advanced Pediatric Thyroid Cancer Therapeutics Clinic, an innovative, collaborative program between CHOP’s Thyroid Center and Developmental Therapeutics Program.
Outlook for thyroid cancer
The long-term outlook for patients with thyroid cancer in childhood or adolescence varies with the type of cancer and the extent to which the cancer has spread beyond the thyroid before diagnosis and treatment. The vast majority of pediatric patients with thyroid cancer are able to live productive and rewarding lives.
Resources to help
Pediatric Thyroid Center Resources
We have created resources, including videos, to help you find answers to your questions and feel confident with the care you are providing your child.

