Hyperhidrosis Surgery for Children
Daniel: It was terrible. I wanted to get rid of it so much.
Carolina: Sometimes I just wanted to be away from people. I didn’t want to deal with it.
Daniel: It was hard to like swing the bat with my sweaty hands. When I’d go to swing, the bat would sometimes fall out of my hands.
Carolina: I used to play piano and that was really difficult for me because my hands would sweat way too much. They would drip in sweat, it would be all over the keys, and it was just really embarrassing.
Sandra, Daniel’s Mother: At night, when I would tuck him in and everything was quiet, he’d always ask me why aren’t my hands like yours? When will it go away? And I could never give him an answer.
Pablo Laje, MD: So, primary hyperhidrosis is a condition of unknown origin in which the patients have excessive sweating in certain areas of their bodies, usually their hands, occasionally their underarms and their feet.
Carolina: The hardest thing about hyperhidrosis by far, in my opinion, was socially with friends. I didn’t know why I had it and why I was different.
Daniel: Writing was hard because when I would like write long stories, the paper would get wet and it would rip up.
Sandra, Daniel’s Mother: The sweat would just pour off his hands on all the papers, puddles on the desk.
Leanne Magee, PhD: Patients with hyperhidrosis can be very self-conscience about their sweating, which can lead them to withdraw from activities that draw attention to it.
Carolina: Having my sweaty hands before was hard because my hands would be sweating and dripping everywhere. So, you could see it, you could see little drops of water coming out of my hands. Like it was really intense.
Sandra, Daniel’s Mother: It did affect his school work. The teachers would write a note, “neater next time,” and it was very upsetting as a parent.
Pablo Laje, MD: CHOP is different than other hospitals when it comes to primary hyperhidrosis in the fact that we take a look at these patients from multiple points of view.
Mary Kate Klarich, MSN, CRNP: We get patients from all over. We’re one of the only centers that is multi-disciplinary for the hyperhidrosis that will perform surgery on children.
Sandra, Daniel’s Mother: It was years of going to the pediatrician and bringing it up repeatedly. They would often say it’s normal. It should go away.
Leanne Magee, PhD: Many of our families had no idea that this was a treatable condition before they came to CHOP and before they ended up here. And this is something that most of these kids live with for years and years.
Mary Kate Klarich, MSN, CRNP: So, we offer them primarily surgical therapy, but we also like them to try medical therapy. So, there’s different things you can do before surgery.
Kali Rhodes, MSN, CRNP: And we do often for the families that may come in and say, “I’m not quite sure if we’re at the point where we would like to discuss surgery.” We may say OK, well, would you like to try something topical on the hands, something you put on your hands, or do you want to try a medicine first? And we’re more than happy to kind of continue to follow them throughout other treatments too.
Alexa: I am getting my surgery for my hyperhidrosis today.
Alexa’s Mother: This has been an issue she’s been dealing with for her whole life really.
Alexa: I’m feeling a little bit nervous. My hopes for today that my hands don’t sweat anymore. My surgeon is Dr. Laje, and I just can’t wait to have dry hands.
Alexa’s Mother: Alexa had a lot of difficulty driving, and that’s when I really began to notice how much of a true issue it was. She would constantly take her hands off the steering wheel and wipe her hands on her shirt or her pants. And to me, it just became a huge safety issue.
Pablo Laje, MD: Good morning.
Alexa: Hi
Pablo Laje, MD: How are you? Hi Alexa, how are you?
Alexa: I’m good.
Pablo Laje, MD: Hi dad, how are you? And mom?
Alexa’s Mother: Hi
Pablo Laje, MD: How is it going?
Alexa: Good. I’m nervous.
Pablo Laje, MD: I’m sure. You’ll find everything will be quick and easy. And so, in a few minutes we’ll be going to the operating room. Mom and dad, you’ll be taken to the waiting room. This will take roughly about an hour.
We have developed a program here along with the dermatology team, the cardiology team, the psychology team, and a dedicated team of nurse practitioners, surgeons and operating room nurses. All patients interview with our pediatric psychologist and all patients are seen by a primary caretaker as well prior to the surgery.
Primary hyperhidrosis occurs because the nerves that innervate and activate the sweat glands of the hands are constantly working and sending signals so that glands will sweat, regardless of the social situation, regardless of the temperature.
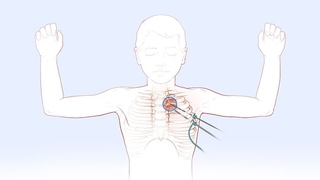
So, the surgery that we’ll do is a minimally invasive procedure that is done through two tiny incisions on each underarm and consists in cutting a little nerve that we have along the spine.
By cutting the nerve that we do for this operation, we do not affect any other innervation in a clinically relevant way. The operation is very safe and the incidence of surgical complications is extremely low, and the effectiveness of the surgery to cure the excessive sweating on the hands is just about 100 percent. The operation can have a potential side effect called compensatory sweating.
Mary Kate Klarich, MSN, CRNP: Compensatory sweating is when your hands might be dry after surgery, but you start sweating somewhere else. And in our numbers, it’s between 2 and 5 percent. So, we haven’t had many cases.
Alexa’s Mother: I’m really excited for her. I’m excited for her to move on to the next phase of her life and to not have to deal with this issue anymore.
Pablo Laje, MD: Hi everybody, how are you?
Alexa’s Dad: Good
Pablo Laje, MD: Alright, we’re all done.
Alexa’s Dad: Excellent
Pablo Laje, MD: Everything went really well.
The recovered time from the surgeries is extremely quick and the results are immediate. So, patients wake up from the anesthesia after the surgery with dry hands forever.
Hello.
Alexa: Like feel my hands.
Pablo Laje, MD: Are they dry?
Alexa: They’re dry.
Alexa’s Mother: That’s all she keeps saying. Her hands are dry.
Pablo Laje, MD: Oh, my God, this is awesome.
Mary Kate Klarich, MSN, CRNP: So, when the children wake up after surgery, they wake, they look down at their hands, they feel them, they notice they’re dry, and then they look up at you with the biggest smile.
Alexa’s Mother: Hi.
Mary Kate Klarich, MSN, CRNP: Because it’s an immediate gratification. One of the best things to see.
Daniel: I felt excited and happy.
Sandra, Daniel’s Mother: He just kept telling us after the surgery, “My hands are dry, my hands are dry, feel my hands,” and he would start holding my hand, which he had never done before.
Carolina: The results were immediate. I woke up and my hands were extremely dry.
Pablo Laje, MD: Prior to the operation, they are very shy and then after the operation, it’s just amazing. They cannot believe the results and their entire life changes.
Leanne Magee, PhD: They’re just feeling much more confident, much more at ease.
Alexa: Right when I woke up, I notice that my hands were dry and I was telling everyone, I was like look, feel my hands, they’re dry.
Carolina: The best thing after my operation was definitely being able to live in the moment, and I’m just doing what I want to do, when I want to do it.
Sandra, Daniel’s Mother: I still can’t believe his hands are fixed and it was what I had always dreamed it would be.
Alexa: Today was a ten for me.