What are esophageal atresia and tracheoesophageal fistula?
Esophageal atresia (EA) and tracheoesophageal fistula (TEF) are rare conditions that develop before birth. They often occur together and affect the development of the esophagus (food pipe), trachea (windpipe) or both. These conditions can be life-threatening and must be treated shortly after birth.
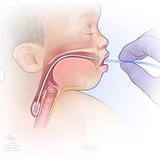
During normal prenatal development, the trachea (the windpipe that connects the throat to the lungs) and the esophagus (the food pipe that connects the back of the mouth to the stomach) start out as a single tube. While babies are developing in the womb, a wall usually forms in the tube. This divides it into two separate tubes that are not connected. The trachea is for air, and the esophagus is for food.
If the esophagus and trachea don’t form correctly or divide completely, an esophageal atresia (EA) and/or tracheoesophageal fistula (TEF) can occur. While EA can appear alone, most forms of EA also include TEF.
What is esophageal atresia?
The esophagus is the tube that carries food from the mouth to the stomach. Esophageal atresia occurs when the esophagus forms in two separate segments (upper and lower) that don’t connect to each other.
As a result, the baby cannot swallow, and food and saliva cannot get from the mouth to the stomach.
What is tracheoesophageal fistula?
In medicine, an abnormal connection is known as a fistula. Tracheoesophageal fistula, also called a TE fistula or TEF, is an abnormal connection in one or more places between the esophagus and the trachea. These abnormal connections can harm a baby’s breathing.
Causes of EA and TEF
The direct cause of EA/TEF is not known. Research suggests there is a genetic component because around half of the babies born with EA or TEF are also born with other health concerns. CHOP’s Genetics team is actively researching the cause of EA/TEF to counsel our families.
Associated conditions
Associated conditions EA/TEF have been linked to include:
- VACTERL association is a complex condition that babies are born with where several health concerns are often seen together that affect the vertebrae (spine), anus, heart (cardiac), trachea, esophagus, kidney (renal), and limbs
- Digestive tract problems such as congenital diaphragmatic hernia, duodenal atresia, or imperforate anus
- Heart problems such as ventricular septal defect, tetralogy of Fallot, or patent ductus arteriosus
- Kidney and urinary tract problems such as horseshoe or polycystic kidney, absent kidney, or hypospadias
- Muscular or skeletal problems
- Trisomy 13, Trisomy 18 and Trisomy 21 (Down syndrome)
Symptoms of esophageal atresia and tracheoesophageal fistula
For babies born with both esophageal atresia (EA) and tracheoesophageal fistula (TEF), symptoms appear almost immediately after birth.
The most common EA and TEF symptoms include:
- Difficulty breathing
- Coughing or choking when swallowing or trying to eat
Babies with esophageal atresia cannot swallow breastmilk, bottled milk or even their own saliva, and food cannot get to their stomach to be digested. To protect the baby from breathing in their saliva, a small tube is placed in the mouth to reach the upper blind pouch. This tube is called a replogle. The tube clears out spit until surgery can be performed.
In the most common type of esophageal atresia with tracheoesophageal fistula, there is a connection between the lower esophagus and the airway. This can be harmful to the baby’s lungs when stomach juices reflux or regurgitate through the connection. Finding the location of a TEF is an early priority in the care of these babies.
In rare cases, a TEF may occur without EA. For these babies, it may take several weeks to diagnose the condition because TEF symptoms usually only appear as mild coughing or respiratory problems. In these cases, babies are still able to successfully swallow and reach their stomach. However, the liquid can leak through the connection from the esophagus to the trachea and get into the lungs. This can cause infections or pneumonia.
Other symptoms of TEF and/or EA can include:
- Frothy, white bubbles coming from the mouth
- Unable to successfully feed by mouth
- Very round, full belly (from gas being trapped there)
- Bluish color to the skin, especially when the baby is eating
- Clinician is unable to pass a tube from the baby’s mouth into their stomach
Diagnosis of EA/TEF
Most babies with esophageal atresia and tracheoesophageal fistula are diagnosed shortly after birth when symptoms first appear. In these cases, clinicians perform a physical examination of the baby, get a medical history, then perform tests to determine how the child’s trachea and esophagus are affected.
Tests may include:
- Rigid bronchoscopy and esophagoscopy: For these tests, a physician uses a telescope and a small camera to look into the baby’s windpipe (trachea) and food pipe (esophagus). This allows us to see how far apart the two parts of the esophagus are from each other. It also shows if there are any connections between the trachea and esophagus. These tests play a very important role in helping doctors pinpoint the specific type of EA/TEF. This is the first step to creating a tailored care plan.
- X-rays with a nasogastric tube: For this test, a clinician will insert a nasogastric tube (NG tube) into the baby’s nose and down the esophagus and try to get it to the stomach. If the NG tube hits a blocked end of the esophagus — which happens if your child has EA – doctors can use X-rays to see the blockage and its location. X-rays can also show if there is gas in your baby’s stomach, which is a sign of a connection between the lower part of the esophagus and the baby’s windpipe.
- Esophagram: If clinicians suspect a baby has TEF without EA, they may have them swallow a liquid contrast or dye. They will then X-ray the child’s upper digestive tract to see if swallowed contrast enters the airway or to identify any other abnormalities
Most babies with EA/TEF are diagnosed after birth. However, as prenatal imaging has improved, some babies with EA/TEF are now being diagnosed before birth with high-resolution fetal ultrasound. At Children’s Hospital of Philadelphia (CHOP), our Center for Fetal Diagnosis and Treatment can help your family prepare for the birth of your baby with EA/TEF and create a treatment plan to address the condition(s) shortly after birth.
Early and thorough evaluation is important. It helps determine which type of EA/TEF your child has, which guides the best treatment approach for each baby’s unique condition.
Treatment for esophageal atresia and tracheoesophageal fistula
If your baby has esophageal atresia (EA) and/or tracheoesophageal fistula (TEF), they will need surgery. In some cases, multiple procedures may be needed. The type of surgery will depend on the following factors:
- The location of the TEF and the impact on the baby’s breathing
- The overall health of your baby, including any heart conditions or prematurity
At CHOP, your child will be cared for by an expert team with experience caring for children with these conditions. Our pediatric surgeons, surgical advanced practice providers and pediatric anesthesiologists offer the most advanced and individualized surgical repair options. Your child will also have access to any other specialists and support they may need. Care can start before birth and will continue throughout childhood and long-term follow-up.
Many children with history of esophageal atresia and tracheoesophageal fistula may benefit from our Esophageal and Airway Treatment (EAT) Program which specializes in diagnosing and treating children with complex esophageal and airway problems. This team brings together experts across many specialties to provide complete, personalized and proactive care for each child.
What to expect during surgery for EA/TEF
At Children’s Hospital of Philadelphia, your baby with EA/TEF will be cared for in the Newborn/Infant Intensive Care Unit (N/IICU) before and after surgery. While your baby is being evaluated and preparing for surgery, they cannot be fed by mouth and are given an IV for nutrition, hydration and any medications they need. The N/IICU staff will also provide your baby with breathing support and additional support for prematurity, if needed.
In some cases, babies with EA or TEF have additional health issues that are part of VACTERL association. This is a group of conditions that can occur together. Tests for a possible VACTERL association will be done at your baby’s bedside in the N/IICU. The tests will tell us if your baby needs extra support from additional specialists for any related conditions. Blood will also be drawn to determine type, electrolyte levels and any signs of infection. If an infection is found, your baby may be given antibiotics.
Preparing for surgery
At the time of EA/TEF surgery, your baby will be given a breathing tube, if they don’t already have one. The breathing tube will help keep their airway open during surgery. A pediatric anesthesiologist will then give them medicine to keep them comfortable for the operation.
Surgery for EA and TEF is performed through an opening on the side of your baby’s chest. Depending on the type of surgery your child needs, either one long opening in the side of the chest will be needed or several small openings.
A bronchoscopy is the first step in repair. In a bronchoscopy, a small camera is put down the windpipe (trachea) to look for fistulas or connections that are small, hidden or not obvious from prior tests. This test helps determine what type of EA and/or TEF your child has.
This key information, plus any other health conditions your child has, will help guide your surgeon as to whether a gastrostomy tube (G tube) is recommended to support nutrition. This tube can also help empty the stomach of extra air or fluid after surgery. For children who have “long-gap" EA (where the two ends of the esophagus are farther apart), a G-tube will be necessary to feed your child before and after their procedures until they are ready to feed by mouth
Stages and types of surgical repair
The specific approach to surgery will depend on the type of EA/TEF your child has, as well as how close the two ends of the esophagus are.
When a connection or fistula is detected between the food pipe (esophagus) and the windpipe (trachea), separating these tubes is usually the first step of surgery. The openings in the food pipe and windpipe are surgically closed and then the next step is determining the best approach for repairing the esophageal atresia.
The main goal of repairing the esophageal atresia is to connect the two ends of the esophagus to create a functioning channel between the back of the throat and the stomach for safe swallowing.
Each child with EA/TEF is on a unique journey to establish safe swallowing and wellness. Some children will need just one surgery known as a “primary repair.” Some children may have planned staged surgeries, while others may have a need for future surgeries to improve the esophagus or trachea as they grow and develop.
- “Primary” repair: Primary repair of esophageal atresia is the typical surgery used for less severe forms of the condition. For example, it is used when the two ends of the esophagus are not very far apart. In some cases, your child’s surgeon may recommend waiting to allow more time for growth before surgery. This gives the esophagus more time to grow closer together, allowing for primary repair.
- Staged surgical repair, also called the Foker process: If the two ends of the esophagus are farther apart (a “long gap”) and have not grown closer together, a staged surgical process may be recommended. It is called “staged” because we break the surgery into stages or steps. Using this approach, surgeons carefully guide the growth of the two ends to bring them together.
- Esophagostomy or “spit fistula:” An opening in the neck or chest is created and connected to the upper esophagus to allow spit to leave the body safely. This may be needed if a primary or staged repair are not possible. Many children with this can also learn to eat for practice while being considered for a replacement of the esophagus.
Recovery and follow-up care after surgery
Once your baby’s EA and/or TEF are repaired, the most important next step is to allow time for healing.
After surgery for EA/TEF, your baby will return to the N/IICU. Depending on your child’s condition and which type of surgery they had, your baby may have an IV for pain medications, a G tube to carry food to the stomach, and/or a chest tube to drain fluid away from their reconnected esophagus.
Your baby may also need a ventilator to help them breathe after surgery. Once your child can breathe on their own, the ventilator will be removed.
The chest tube (drain) will stay in place until a week or two after surgery. At that time, we will do special tests to make sure the repair is complete and successful and there are no leaks. These tests include:
- Esophagram - This is a special study that uses contrast or dye. The dye is either given by mouth or through a small feeding tube and then is visible on X-ray. The dye helps to show if there are any leaks and make sure the esophagus has healed well. If a leak is found, the drain will stay in place until the leak stops.
- Esophagoscopy (EGD) - This is a test that uses a small camera to look inside the esophagus. EGD studies will be repeated after esophageal repair to check on the healing of the esophagus. The EGD can also allow for gentle stretching (dilation) of the esophagus and collect tissue samples. Your baby’s GI doctor or endoscopist will help you plan for getting this test after surgery and after your baby is discharged home from the hospital.
Your baby will not be able to eat by mouth until they have healed after surgery. Most babies first receive nutrition through the G-tube as they practice eating smaller amounts by mouth. It can take a while for babies with EA/TEF to work up to eating everything by mouth.
When can my baby go home after surgery?
The timing of your baby’s discharge after surgery will depend on many things, including:
- Whether your baby was born prematurely
- If your baby’s esophagus could be connected right away
- Your baby’s respiratory status
- Whether other medical problems were identified in your baby
If your baby was born prematurely, they will likely need to remain in the hospital for several weeks or even months after surgery. Your baby may only need to be hospitalized for a few weeks if:
- Your baby was close to full term
- The esophagus could be connected right away
- There was not a leak after the esophagus was repaired
Before your child is discharged from the hospital, you will be taught how to:
- Feed your baby if they have a feeding tube
- Give your baby medications, if needed
- Mix formula or breast milk if your baby needs increased calories
- Take care of your baby’s incision and dressing, if applicable
You’ll also be taught how to spot signs of possible respiratory infection or narrowing of the esophagus, and when to call the pediatrician or surgeon with concerns or problems.
Support for ongoing challenges
Every child’s EA/TEF diagnosis and treatment is unique. Your care team will be here to support you and your family during your journey.
- Eating by mouth: This is often a priority for families, and is often possible, but may take ongoing support from dietitians and speech therapists.
- Gastroesophageal reflux (GER). This is very common after EA/TEF surgery. It is treated with medications prescribed by the surgical/medical team (or, rarely, with an operation called a fundoplication).
- Esophageal stricture: Scar tissue at the surgical site causes the esophagus to narrow. This may make it more difficult for your baby to swallow food. This is treated by a procedure to widen (also called dilate) the esophagus.
- Tracheomalacia, also known as a “floppy airway” is a wider shaped windpipe with a flexible backwall. All babies with EA/TEF history have some degree of tracheomalacia ranging from mild to severe. This causes collapse of the windpipe with increased airflow, such as coughing or crying. Because of this, your baby’s cry or cough may sound like a “barking” sound similar to a seal or a sea lion. This collapse can make it more difficult for children to clear the mucous or secretions from their lungs. Mild tracheomalacia may be cared for with nebulizers and close Pulmonary follow-up. Surgery is reserved for the most severe tracheomalacia cases.
Follow-up care for EA/TEF
Children’s Hospital of Philadelphia is dedicated to caring for your child and your family through this unique journey with EA/TEF. Your team will guide you through any testing needed after surgery and support your child with feeding and nutrition as well as your baby’s airway and respiratory health.
A few weeks after your baby leaves the hospital, they will need to come back for a follow-up visit. Your child’s surgeon will make sure the incision is healing and your baby is recovering and growing as expected. Support staff will help your family coordinate additional services. These may include home nursing visits, early intervention services, speech therapy, physical therapy, and occupational therapy, as needed.
Based on your child’s unique needs, they may be referred to the Esophageal and Airway Treatment Program which brings together General Surgery, Gastroenterology, Pulmonology, Otolaryngology (ENT), Nutrition, and Speech and Language Pathology in one location at CHOP’s Philadelphia Campus. Additional follow-up care and ongoing support and services are available primarily in Philadelphia, with select specialty care throughout the CHOP Care Network. Our team is committed to partnering with you to provide the most current, comprehensive, and specialized care possible for your child.
Long-term outlook for esophageal atresia and tracheoesophageal fistula
Children with a history of EA and TEF are able to thrive after leaving the hospital with the help of a dedicated healthcare team.
Many children with EA/TEF can learn to eat by mouth with the support of surgical dietitians and speech therapists along the way. Children with EA/TEF history should be monitored closely for their growth, respiratory health, signs of gastroesophageal reflux (GER) and strictures through all their stages of development. Partnership through common childhood respiratory illnesses is key for children with EA/TEF history and associated tracheomalacia.
We are here to support your child and your family along this journey each step of the way.

Why choose CHOP for your child's surgery
If your child needs surgery, you want to know their care is in the hands of the best, most compassionate team. CHOP's world-class pediatric surgeons and experienced staff are here for you.

Preparing for surgery
Find tips to prepare for your preoperative visit with CHOP’s pediatric general surgeons, and resources to help prepare your child for surgery.
Resources to help
Division of Pediatric General, Thoracic and Fetal Surgery Resources
We have created resources to help you find answers to your questions and feel confident with the care you are providing your child.





