
When it comes to effectively and safely treating children with congenital hyperinsulinism (HI), one key member of the Congenital Hyperinsulinism Center team looms large for about a quarter of the patients: Lisa J. States, MD, a pediatric radiologist and nuclear medicine specialist.
Of all the patients who have hyperinsulinism (HI), about half can have their disease managed by medication. The other half face surgery to have most or part of their pancreas removed to control the excess insulin secretion that cause extremely low — and dangerous — blood glucose levels.
Genetic testing plays a pivotal role in determining if the child has diffuse HI, when abnormal insulin-secreting beta cells are present throughout the pancreas, or focal HI, when only a small cluster of beta cells (a marble-like lesion) is in one part of the pancreas. The difference is huge, as children with focal HI can be cured after resection of the lesion. The remaining pancreas is normal. Resection leads to a cure 97% of the time at the CHOP HI Center.
It is Dr. States who works with other members of the HI Center team to determine which HI patients being treated at CHOP may have focal HI and will therefore benefit from advanced imaging to better locate the focal area in the pancreas. Knowing the site of the lesion in advance makes the surgery less complicated and safer.
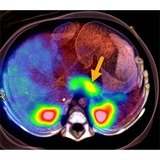
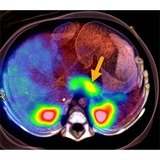
The 18F-L-Fluoro-DOPA PET/CT scan, which can identify where the lesion is located within the pancreas, was initially pioneered at the Hospital of the University of Pennsylvania (HUP) by Abass Alavi, MD, and transferred to CHOP under the leadership of Charles Stanley, MD, founder of CHOP’s HI Center. Over 460 18F-L-Fluoro-DOPA PET/CT scans have been performed at CHOP, more than at any other hospital in the United States.
Dr. States explains the 18F-DOPA PET/CT procedure to families, is present during the scans and then uses her 14 years of experience interpreting the images from the scans to arm Surgeon-in-Chief N. Scott Adzick, MD, MMM, with the best information to guide the surgery to remove the focal lesion.
“The imaging is important for surgical planning,” Dr. States says. “I provide Dr. Adzick with detailed anatomical descriptions, which are critical, especially if he can’t see or feel the lesion during surgery because it is in a position behind the pancreatic body, deep in the pancreatic head or in an otherwise hidden place, like behind the vessels leading to the spleen.”
How does the PET scan work?
Once the HI Center team has determined the child has focal HI, Dr. States will meet with the family to go over each detail and get the consent forms signed.
On the day of the scan, the 18F-L-Fluoro-DOPA — the radioactive tracer that will locate the overactive beta cells — is produced next door to CHOP in the cyclotron at HUP, CHOP’s long-time partner for this test. There is a limited amount of time between when the 18F-DOPA is synthesized and when it must be used for the scans, making the close proximity a plus.
The child’s glucose level is checked soon before the scan and, if needed, is raised with additional dextrose, as levels must be in the target range during the procedure. The child is sedated by an experienced pediatric anesthesiologist and positioned in the combination PET/CT scanner. Then Dr. States injects the 18F-DOPA via an intravenous (IV) line over about one minute. The dose depends on the baby’s weight. With the combo equipment, the child does not need to be moved during the scanning. The PET scan is first and takes about an hour. A contrast-enhanced CT scan follows and takes only a few minutes.
The PET and CT scans images are fused together by a computer to give the most accurate “map” of the potential location of the lesion. Dr. States then reads the scans and shares her findings with the rest of the HI team, and Dr. Adzick plans the surgery.
Sometimes, the lesion doesn’t pop on the scan
There are times when the PET/CT scan does not reveal the location of the focal lesion. This happens in about 15% of PET/CT scans, usually because the lesion is 5 mm or smaller (less than one-quarter of an inch) or is flat or ribbon shaped. Radiology can play a role in these cases, too.
Because the child’s HI can’t be adequately managed by medication, surgery is still scheduled. With more than 609 pancreatectomies performed, Dr. Adzick is incredibly skilled at finding the lesion on the rare occasions he’s working without the roadmap of the 18F-DOPA PET/CT.
He looks for color or structural differences that could signal its location. He palpates the pancreas and has found many lesions by feel. He also takes numerous biopsies of pancreatic tissue, which are immediately examined by a pathologist, looking for the signs of lesion cells among normal pancreatic cells.
Dr. States or one of her Radiology colleagues will be in the operating room, ready to use intraoperative ultrasound (US) as another way to locate the lesion. Using an US probe shaped like a tiny hockey stick, the radiologist will search the surgical area for the elusive lesion so it can be removed.
History and future of 18F-DOPA PET/CT
CHOP’s HI Center has led the use of 18F-DOPA PET/CT in the United States to pinpoint the location of focal lesions and began performing these scans in 2004. Because the U.S. Food and Drug Administration has not approved the use of 18F-FDOPA in children (although the European Union has), tests performed at CHOP are done under an FDA-authorized investigational new drug application and institutional review board-approved protocol.
Dr. States is part of a group of radiologists, nuclear medicine specialists and researchers that has petitioned the FDA to officially recognize the invaluable information an 18F-DOPA PET/CT scan can bring to the care of a child with focal HI and to recognize its safety for this use.
As the leader — with more than four times more scans performed than any other pediatric institution — CHOP continues to be a magnet for families seeking expertise in curing focal HI.
“A confluence of factors has allowed CHOP to be in the position to help these children,” Dr. States says. “The HI Center team has been at the forefront of HI care for over 50 years, and our team keeps working to push the boundaries of treatment. CHOP as an institution has been supportive, launching the center and buying the equipment we need. Together, we know we can provide children with HI with the best possible outcomes. We could not offer these scans without the support of the HUP cyclotron and our experienced CHOP nuclear medicine technologists.”
Featured in this article
Specialties & Programs

When it comes to effectively and safely treating children with congenital hyperinsulinism (HI), one key member of the Congenital Hyperinsulinism Center team looms large for about a quarter of the patients: Lisa J. States, MD, a pediatric radiologist and nuclear medicine specialist.
Of all the patients who have hyperinsulinism (HI), about half can have their disease managed by medication. The other half face surgery to have most or part of their pancreas removed to control the excess insulin secretion that cause extremely low — and dangerous — blood glucose levels.
Genetic testing plays a pivotal role in determining if the child has diffuse HI, when abnormal insulin-secreting beta cells are present throughout the pancreas, or focal HI, when only a small cluster of beta cells (a marble-like lesion) is in one part of the pancreas. The difference is huge, as children with focal HI can be cured after resection of the lesion. The remaining pancreas is normal. Resection leads to a cure 97% of the time at the CHOP HI Center.
It is Dr. States who works with other members of the HI Center team to determine which HI patients being treated at CHOP may have focal HI and will therefore benefit from advanced imaging to better locate the focal area in the pancreas. Knowing the site of the lesion in advance makes the surgery less complicated and safer.
The 18F-L-Fluoro-DOPA PET/CT scan, which can identify where the lesion is located within the pancreas, was initially pioneered at the Hospital of the University of Pennsylvania (HUP) by Abass Alavi, MD, and transferred to CHOP under the leadership of Charles Stanley, MD, founder of CHOP’s HI Center. Over 460 18F-L-Fluoro-DOPA PET/CT scans have been performed at CHOP, more than at any other hospital in the United States.
Dr. States explains the 18F-DOPA PET/CT procedure to families, is present during the scans and then uses her 14 years of experience interpreting the images from the scans to arm Surgeon-in-Chief N. Scott Adzick, MD, MMM, with the best information to guide the surgery to remove the focal lesion.
“The imaging is important for surgical planning,” Dr. States says. “I provide Dr. Adzick with detailed anatomical descriptions, which are critical, especially if he can’t see or feel the lesion during surgery because it is in a position behind the pancreatic body, deep in the pancreatic head or in an otherwise hidden place, like behind the vessels leading to the spleen.”
How does the PET scan work?
Once the HI Center team has determined the child has focal HI, Dr. States will meet with the family to go over each detail and get the consent forms signed.
On the day of the scan, the 18F-L-Fluoro-DOPA — the radioactive tracer that will locate the overactive beta cells — is produced next door to CHOP in the cyclotron at HUP, CHOP’s long-time partner for this test. There is a limited amount of time between when the 18F-DOPA is synthesized and when it must be used for the scans, making the close proximity a plus.
The child’s glucose level is checked soon before the scan and, if needed, is raised with additional dextrose, as levels must be in the target range during the procedure. The child is sedated by an experienced pediatric anesthesiologist and positioned in the combination PET/CT scanner. Then Dr. States injects the 18F-DOPA via an intravenous (IV) line over about one minute. The dose depends on the baby’s weight. With the combo equipment, the child does not need to be moved during the scanning. The PET scan is first and takes about an hour. A contrast-enhanced CT scan follows and takes only a few minutes.
The PET and CT scans images are fused together by a computer to give the most accurate “map” of the potential location of the lesion. Dr. States then reads the scans and shares her findings with the rest of the HI team, and Dr. Adzick plans the surgery.
Sometimes, the lesion doesn’t pop on the scan
There are times when the PET/CT scan does not reveal the location of the focal lesion. This happens in about 15% of PET/CT scans, usually because the lesion is 5 mm or smaller (less than one-quarter of an inch) or is flat or ribbon shaped. Radiology can play a role in these cases, too.
Because the child’s HI can’t be adequately managed by medication, surgery is still scheduled. With more than 609 pancreatectomies performed, Dr. Adzick is incredibly skilled at finding the lesion on the rare occasions he’s working without the roadmap of the 18F-DOPA PET/CT.
He looks for color or structural differences that could signal its location. He palpates the pancreas and has found many lesions by feel. He also takes numerous biopsies of pancreatic tissue, which are immediately examined by a pathologist, looking for the signs of lesion cells among normal pancreatic cells.
Dr. States or one of her Radiology colleagues will be in the operating room, ready to use intraoperative ultrasound (US) as another way to locate the lesion. Using an US probe shaped like a tiny hockey stick, the radiologist will search the surgical area for the elusive lesion so it can be removed.
History and future of 18F-DOPA PET/CT
CHOP’s HI Center has led the use of 18F-DOPA PET/CT in the United States to pinpoint the location of focal lesions and began performing these scans in 2004. Because the U.S. Food and Drug Administration has not approved the use of 18F-FDOPA in children (although the European Union has), tests performed at CHOP are done under an FDA-authorized investigational new drug application and institutional review board-approved protocol.
Dr. States is part of a group of radiologists, nuclear medicine specialists and researchers that has petitioned the FDA to officially recognize the invaluable information an 18F-DOPA PET/CT scan can bring to the care of a child with focal HI and to recognize its safety for this use.
As the leader — with more than four times more scans performed than any other pediatric institution — CHOP continues to be a magnet for families seeking expertise in curing focal HI.
“A confluence of factors has allowed CHOP to be in the position to help these children,” Dr. States says. “The HI Center team has been at the forefront of HI care for over 50 years, and our team keeps working to push the boundaries of treatment. CHOP as an institution has been supportive, launching the center and buying the equipment we need. Together, we know we can provide children with HI with the best possible outcomes. We could not offer these scans without the support of the HUP cyclotron and our experienced CHOP nuclear medicine technologists.”
Contact us
Congenital Hyperinsulinism Center