Division of Endocrinology and Diabetes

At the Division of Endocrinology and Diabetes at Children's Hospital of Philadelphia (CHOP), we understand how endocrine disorders can impact your child's growth and development, as well as contribute to the onset of diabetes. Our team of experts is here to assess your child, offer accurate diagnosis and provide advanced treatment options for a wide range of endocrine disorders.

U.S. News & World Report ranked CHOP the No. 1 children’s hospital for pediatric endocrinology care in the country for 2024-2025. We are also ranked among the best pediatric endocrinology programs in the nation by Newsweek.
We are one of the largest pediatric endocrinology centers in the nation and have expertise in many endocrine conditions including:
- Thyroid, adrenal and pituitary disorders
- Calcium, bone health and mineral metabolism disorders
- Diabetes
- Hyperinsulinism and other hypoglycemia disorders
See how we can help your child.
How we serve you
Whether your child has a common or rare diagnosis, we have experts who can help. Our numerous programs and specialty clinics focus on specific endocrine disorders. These programs include additional specialists who work closely with our pediatric endocrinologists and are available to treat your child, if needed.
-
Adrenal and Puberty Center -
Advanced Pediatric Thyroid Cancer Therapeutics Clinic -
Center for Bone Health -
Congenital Adrenal Hyperplasia Program -
Congenital Hyperinsulinism Center -
Diabetes Center -
Diabetes: Transitioning to Adulthood -
ELECT Program -
Endocrinology Second Opinion Program -
Fine Needle Aspiration -
Glycogen Storage Disease Clinic -
Growth Center (Diagnostic and Research) -
Klinefelter Program -
Monogenic and Atypical Diabetes Program -
Neuroendocrine Center -
Pediatric Thyroid Center -
Polycystic Ovarian Syndrome Clinic -
Pseudotumor Cerebri Collaborative Clinic -
STRIVE for Kids Program -
Turner Syndrome Center
Conditions we treat
We pride ourselves on understanding the complexities of common conditions and knowing the latest research on rare diseases. See the many conditions our experts treat:
-
Adrenal insufficiency -
Ambiguous genitalia -
Central nervous system (CNS) germ cell tumors -
Childhood craniopharyngioma -
Congenital adrenal hyperplasia -
Congenital hyperinsulinism (HI) -
Cushing’s syndrome -
Cystic fibrosis-related diabetes -
Delayed puberty -
22q11 deletion (DiGeorge) syndrome -
Diabetes insipidus -
Differentiated thyroid cancer -
Early (precocious) puberty -
Empty sella syndrome -
Ectopic posterior pituitary - Endocrine late effects after cancer therapy
-
Generalized arterial calcification of infancy (GACI) -
Graves’ disease -
Glycogen storage disease -
Growth hormone deficiency -
Hypercalcemia -
Hypocalcemia -
Hyperthyroidism -
Hypothalamic obesity -
Hypothalamic hamartoma -
Hypothyroidism -
Kallmann syndrome -
Ketotic hypoglycemia -
Klinefelter syndrome -
Low bone density and osteoporosis -
Lipodystrophy -
Medullary thyroid cancer -
Monogenic and atypical diabetes -
Multiple endocrine neoplasia (MEN) syndrome type 1 -
Multiple endocrine neoplasia (MEN) syndrome type 2 -
Noonan syndrome -
Osteogenesis imperfecta in children -
Panhypopituitarism in children -
Postprandial hypoglycemia -
Pituitary cysts -
Pituitary tumors - Postpancreatectomy diabetes
- Prader willi syndrome
-
Prolactinoma -
Pseudotumor cerebri syndrome (PTCS) -
Polycystic ovary syndrome (PCOS) -
Rickets -
Septo-optic dysplasia - Short stature
-
Thyroid cancer -
Thyroid nodules -
Type 1 diabetes -
Type 2 diabetes -
Turner syndrome

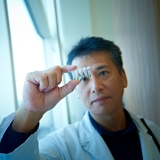
Meet your team
Our experienced teams of pediatric endocrinologists, nurses, social workers and psychologists bring their disease-specific expertise to the care of children with a broad range of endocrinology disorders.

Our locations
Access endocrinology and diabetes care in one of our many regional locations.
Our research
We are continually researching and innovating in the field of endocrinology, better understanding the causes of endocrine disease and how they can be best treated.

Division of Endocrinology and Diabetes resources
We have gathered resources to help you find answers to your endocrine questions.

Resources for professionals
We offer resources for referring physicians, other professionals in the field, and those in training for their career in medicine.
Events
Keeping Kids with Diabetes Safe in School and Community Settings
Saturday, Oct 25, 2025
Your donation changes lives
A gift of any size helps us make lifesaving breakthroughs for children everywhere.


