Division of Pediatric General, Thoracic and Fetal Surgery

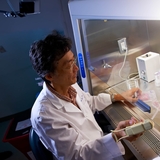
Learning that your child needs surgery can be frightening. You likely have a lot of questions about the procedure they need and the next steps. Find the answers and support you and your child need from our team of experts at the Division of Pediatric General, Thoracic and Fetal Surgery at Children's Hospital of Philadelphia (CHOP). We are considered one of the best hospitals for pediatric surgery in the world. Families fly from around the country and the world for our surgical expertise. Each member of our team is specially trained to care for children with a variety of conditions that require surgery.
How we serve you
Our world-class pediatric surgeons and anesthesiologists are experts in performing the full range of surgical procedures. They are always trying to find new and better ways to treat kids with the fewest possible side effects. After surgery, we monitor your child's long-term health through regular follow-up appointments.
-
Esophageal and Airway Treatment (EAT) Program -
About ECMO -
Intestinal Rehabilitation Program -
Center for Lymphatic Disorders -
Minimally Invasive Pediatric Surgery -
Breast Program -
Colorectal Program -
Surgical Oncology Program -
Pediatric Thyroid Surgery -
Vascular Surgery & Endovascular Therapy -
Pulmonary Hypoplasia Program -
Fetal Diagnosis and Treatment -
Trauma Center
Conditions we treat
If your child needs surgery, we are here for you. We are able to provide surgical care for the full range of conditions.
-
Appendicitis in children -
Arterial aneurysms in children and teens -
Biliary atresia -
Branchial cleft abnormalities -
Breast and chest wall disorders -
Bronchopulmonary sequestration (BPS) -
CCAM/CPAM: Congenital cystic adenomatoid malformation (pulmonary airway malformation) -
Choledochal cysts and other biliary malformations -
Congenital diaphragmatic hernia (CDH) -
Conjoined twins -
Crohn's disease -
Dermoid cyst -
Esophageal atresia and tracheoesophageal fistula (EA/TEF) -
Fetal giant neck masses -
Fetal lung lesions -
Gallstones -
Gastroesophageal reflux disease (GERD) -
Gastroschisis -
Hirschsprung's disease -
Hybrid lesions -
Hydrocele -
Hyperhidrosis -
Hyperthyroidism -
Imperforate anus/Anorectal malformation -
Inflammatory Bowel Disease -
Inguinal hernia -
Intestinal malrotation and volvulus -
Intussusception -
Meckel's diverticulum -
Meconium ileus -
Myasthenia gravis -
Omphalocele -
Pectus carinatum -
Pectus excavatum -
Pediatric renovascular hypertension -
Pilomatrixoma -
Pilonidal cysts and sinuses -
Pyloric stenosis -
Sacrococcygeal Teratoma (SCT) -
Small bowel atresia (Intestinal atresia) -
Spontaneous pneumothorax -
Thoracic outlet syndrome in children and teens -
Thyroglossal duct cyst -
Thyroid nodules -
Ulcerative colitis in children -
Umbilical hernia -
Undescended testes

Why choose CHOP for your child's surgery
When your child needs surgery, you want to know their care is in the best hands. Our world-class pediatric surgeons and experienced staff take a multidisciplinary approach to the treatment and care of your child.

Meet your team
Here at the Division of General, Thoracic and Fetal Surgery, you have access to world-class pediatric surgeons who are experts in meeting children’s unique surgical needs. Our surgical team is extensive.

General surgery locations
The location of your child's procedure will depend on the type of surgery they need. You may be able to have the procedure done at one of our Specialty Care and Surgery Centers.
Our research
Over the course of our department's history, our mission has remained the same: developing innovative and minimally invasive procedures, and discovering the latest solutions in pediatric surgical care.

Division of Pediatric General, Thoracic and Fetal Surgery resources
We have created resources to help you find answers to your questions and feel confident with the care you are providing your child.

Resources for professionals
Everything you need to support your patient’s health, created and updated by our CHOP community of experts.

Preparing your child for surgery
If your child is having a surgical procedure performed by one of our pediatric general surgeons, knowing what to expect can help you prepare and put you and your child at ease.

